Cancer Cell:肿瘤细胞种子土壤学说被阐释
2014-05-27 MedSci MedSci原创
最近,中山大学孙逸仙纪念医院乳腺肿瘤中心教授宋尔卫团队的最新研究成果解答了一个百年多来困扰医学界的“种子土壤学说”问题。该项研究近日在国际肿瘤学顶级杂志《癌细胞》上正式发表。“种子土壤学说”,即肿瘤细胞“种子”的生长,需要合适的肿瘤微环境的“土壤”。而恶性肿瘤的“种子”是否会反过来影响其生长的“土壤”,形成促进肿瘤转移的恶性循环呢?宋尔卫教授课题组通过乳腺癌细胞株和人原代巨噬细胞共培养模型,首次揭
最近,中山大学孙逸仙纪念医院乳腺肿瘤中心教授宋尔卫团队的最新研究成果解答了一个百年多来困扰医学界的“种子土壤学说”问题。该项研究近日在国际肿瘤学顶级杂志《癌细胞》上正式发表。
“种子土壤学说”,即肿瘤细胞“种子”的生长,需要合适的肿瘤微环境的“土壤”。而恶性肿瘤的“种子”是否会反过来影响其生长的“土壤”,形成促进肿瘤转移的恶性循环呢?
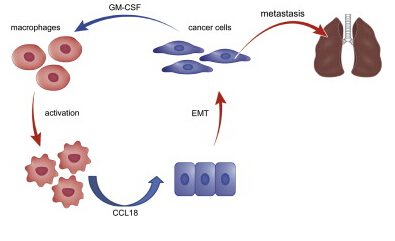
宋尔卫教授课题组通过乳腺癌细胞株和人原代巨噬细胞共培养模型,首次揭示发生了EMT的乳腺癌细胞比未发生EMT的乳腺癌细胞更具有激活巨噬细胞的优势;炎症因子芯片检查发现,发生EMT的乳腺癌细胞通过分泌细胞因子GM-CSF,以及大量代谢产物乳酸,共同激活巨噬细胞;而巨噬细胞又可分泌趋化因子CCL18诱导乳腺癌细胞发生EMT和分泌细胞因子GM-CSF,从而形成恶性循环环路。
该研究阐明了在非可控性炎症微环境中,肿瘤细胞可塑性与炎症细胞激活状态之间的互动机制;为发展针对肿瘤微环境的乳腺癌新型靶向药物提供了实验依据,特别是对内分泌治疗和Her2靶向治疗均不敏感的三阴性乳腺癌的治疗提供了新靶点。
此外,该研究发现乳腺癌细胞发生EMT时,IL-8、GROs等细胞因子表达升高,这些细胞因子对肿瘤血管形成、粒细胞浸润等肿瘤微环境改变具有重要调控作用,这为乳腺癌转移机制的深入探索和治疗新靶标的发现提供了新思路。
原始出处:
Shicheng Su, Qiang Liu, Jingqi Chen, Jianing Chen, Fei Chen, Chonghua He, Di Huang, Wei Wu, Ling Lin, Wei Huang, Jin Zhang,Xiuying Cui, Fang Zheng, Haiyan Li, Herui Yao, Fengxi Su, Erwei Song. A Positive Feedback Loop between Mesenchymal-like Cancer Cells and Macrophages Is Essential to Breast Cancer Metastasis. Cancer Cell, 12 May 2014; DOI: 10.1016/j.ccr.2014.03.021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Cell#
54
#CEL#
41
#cancer cell#
47
#肿瘤细胞#
49
为真正搞科研的中国人赞一个!也对我的研究起了很大启示作用!
126