Cell:垃圾RNA在细胞应激反应中发挥重要作用
2016-12-18 佚名 生物谷
在一项新的研究中,来自美国麻省总医院的研究人员发现了之前被认为是非功能性的“垃圾”RNA分子的一种意想不到的作用:控制细胞对应激作出的反应。他们描述了之前已知抑制基因转录的两个组分---B2 RNA和作为一种之前已知仅沉默基因的酶,EZH2---之间的一种高度特异性的相互作用实际上诱导小鼠细胞应激反应基因表达。相关研究结果发表在2016年12月15日那期Cell期刊上,论文标题为“Destabil
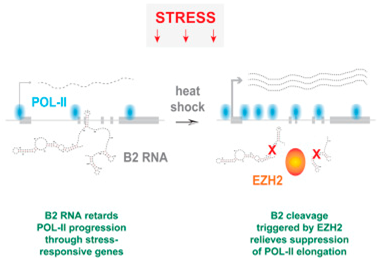
论文通信作者、麻省总医院分子生物学系Jeannie T. Lee博士说,“EZH2是一种被称作多梳抑制复合物2(Polycomb Repressive Complex 2, PRC2)的结构的一部分,其中PRC2沉默靶基因。但是这个领域存在的一个大的悖论是EZH2在有活性的基因和没有活性的基因中都可发现到。我们首次证实EZH2能够在PRC2复合物外面发挥作用:通过另一种机制激活基因---在这项研究中是通过切割B2 RNA来实现的,这种切割随后激活应激反应基因。”
仅不到2%的哺乳动物基因组编码蛋白,而且多年来,人们曾认为非编码性DNA是没有用处的。尽管一些非编码性DNA可转录为维持和调节细胞功能所需的RNA分子---比如tRNA和microRNA,但是认为大多数非编码性RNA没有功能的观点持续存在。这对于长链非编码RNA(lncRNA)而言尤为适用,而且更多的情形是非编码性RNA是由“寄生性”逆转录转座子(retrotransposon)---插入整个基因组中的重复性DNA序列---经过转录而产生的。但是最近在小鼠细胞中开展的研究已表明由B2逆转录转座子经过转录而产生的B2 RNA结合到应激基因上,抑制它们的转录。
Lee团队成员之前的研究已发现9000多种细胞核转录本结合到EZH2上。它还提示着EZH2与一些重复性RNA---包括由逆转录转座子经过转录而产生的RNA---相互作用,但是在当时,B2 RNA和EZH2之间的结合是否真地存在仍是不清楚的。当前的这项研究旨在探究这种结合是否是真的和有功能性的。他们的实验证实EZH2结合到B2 RNA上,而且当遭受热应激时,还会切割这种RNA分子。切割B2 RNA---当未切割时结合到让细胞避免遭受热休克损伤的基因上,从而关闭这些基因---允许转录这些热休克基因。
Lee说,“我们的发现提示着B2 RNA是一种关键的应激反应调节物,而且很可能在所有细胞类型中发挥着这样的作用。我们和其他人是在小鼠体内研究B2细胞,但是这些同样类型的短分散核元件(short interspersed nuclear element, SINE)也在人细胞中发现到,其中在人细胞中,它们存在相当大的不同。尽管人SINE是否具有类似的性质还仍然有待观察,但是如果它们确实发挥这样的作用,我也不会感到吃惊。”
进一步的研究将探究EZH2被招募到应激基因上的特异性机制和它如何切割B2 RNA分子。鉴于这些细胞应激反应抵抗一些重要的疾病,而且有时还在治疗上加以诱导---比如,阻断癌细胞增殖,因此加深对这种应激反应的理解可能对人类健康作出重要的贡献。
Athanasios Zovoilis, Catherine Cifuentes-Rojas, Hsueh-Ping Chu, Alfredo J. Hernandez, Jeannie T. Lee.Destabilization of B2 RNA by EZH2 Activates the Stress Response.Cell.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#应激反应#
70
#Cell#
50
#重要作用#
65
#CEL#
51
#应激#
56