乳腺癌新药3期临床疗效显著,已向FDA提交新药申请
2016-07-24 佚名 药明康德
今天,总部位于美国洛杉矶的生物技术公司 Puma Biotechnology 宣布了最新补充的积极3期临床试验(ExteNET trial)结果,在该项研究中使用其在研新药来那替尼(neratinib)延长性辅助治疗早期HER2阳性反应的乳腺癌患者。同时,基于这些良好的3期(ExteNET)结果,Puma 向美国FDA提交了一份有关来那替尼的新药申请(NDA)

今天,总部位于美国洛杉矶的生物技术公司 Puma Biotechnology 宣布了最新补充的积极3期临床试验(ExteNET trial)结果,在该项研究中使用其在研新药来那替尼(neratinib)延长性辅助治疗早期HER2阳性反应的乳腺癌患者。同时,基于这些良好的3期(ExteNET)结果,Puma 向美国FDA提交了一份有关来那替尼的新药申请(NDA),可用于延长性辅助治疗已经先前接受过曲妥珠单抗(trastuzumab) 辅助治疗的早期HER2过度表达的乳腺癌病人。

众所周知,乳腺癌是威胁全世界女性健康的第一恶性肿瘤,而HER2阳性乳腺癌更是其中最凶险的类型之一。HER2又名“人类表皮生长因子受体2”,乳腺癌HER2阳性其实意味着病人体内的表皮生长因子受体2过度表达,这种被激活的蛋白质可传递信号,刺激癌细胞疯狂增殖。相较于其它类型的乳腺癌,HER2阳性乳腺癌患者对内分泌治疗不敏感、进展速度更快、恶性程度更高,同时也更容易复发和转移,由于化疗效果不理想,预后情况也相对更差。HER2阳性的乳腺癌患者术后复发风险也远高于其他人群。

据世界卫生组织统计,中国每年有16.9万患者被新确诊为乳腺癌,其中,20%~30%的人群罹患的便是HER2阳性乳腺癌。目前的治疗方案包括了使用曲妥单抗辅助治疗,它可导致HER2阳性早期乳腺癌患者复发率下降,但是临床上仍希望能尝试进一步降低疾病的复发风险,进而改善预后。
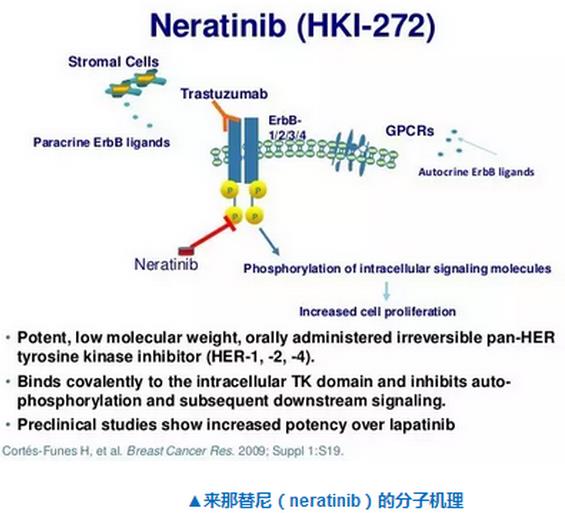
来那替尼是一种有效的不可逆的酪氨酸激酶抑制剂,阻止通过表皮生长因子受体,HER1,HER2和HER4信号通路转导。Puma Biotechnology 向美国FDA提交来那替尼的NDA是基于上述名为ExteNET的双盲、安慰剂对照、3期试验,结果表明应用来那替尼能够进一步改善这种疾病的患者预后。该ExteNET试验在41个国家随机招募了2840例早期HER2阳性乳腺癌患者。该研究的主要终点为无病生存期(DFS),结果表明,与安慰剂相比,来那替尼使无病生存期改善33%,具有统计学上的显著差异(HR = 0.67; P = 0.0046)。

Puma的总裁兼首席执行官Alan H. Auerbach 先生评论说道:“我们非常高兴地宣布这一重要的监管里程碑。我们致力于进一步降低HER2阳性乳腺癌患者的复发风险,相信来那替尼或许能够提进一步帮助这些患者。我们期待着在NDA提交的审查期间与FDA紧密合作。”
该公司认为,来那替尼在治疗其他几个癌症的临床应用也很有潜力,包括HER2过度表达或存在突变的非小细胞肺癌等其他类型肿瘤。
参考资料:
[1] Puma Biotech (PBYI) Announces Interim 5-Year Disease Free Survival Data From Phase III Trial Of PB272 (Neratinib) In Extended Adjuvant HER2-Positive Early Stage Breast Cancer (Extenet Trial)
[2] Puma Biotech (PBYI) Submits New Drug Application For PB272 (Neratinib) To U.S. FDA For Extended Adjuvant Treatment Of HER2-Positive Early Stage Breast Cancer
[3] Puma Biotech 官方网站
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#3期临床#
0
#临床疗效#
59
好文,从这里学习了好多新知识,新信息。赞了!
79
#新药申请#
57
不错不错!
111