Clin Cancer Res:PD-1抗体Geptanolimab治疗罕见肺泡软组织肉瘤的活性
2020-11-07 星云 MedSci原创
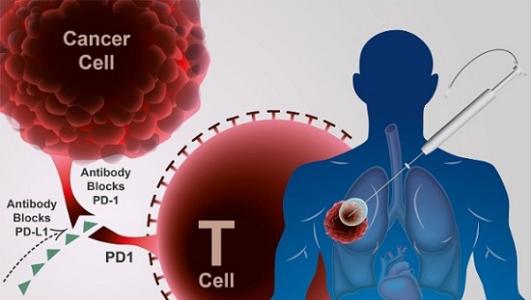
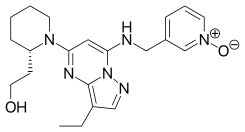
肺泡软组织肉瘤(ASPS)是一种罕见的疾病,治疗方法也少。该研究评估了geptanolimab (GB226),一种完全人源化的程序性细胞死亡蛋白1抗体,用于不可切除的、复发或转移性ASPS患者的活性
肺泡软组织肉瘤(ASPS)是一种罕见的疾病,治疗方法也少。该研究评估了geptanolimab (GB226),一种完全人源化的程序性细胞死亡蛋白1抗体,用于不可切除的、复发或转移性ASPS患者的活性。
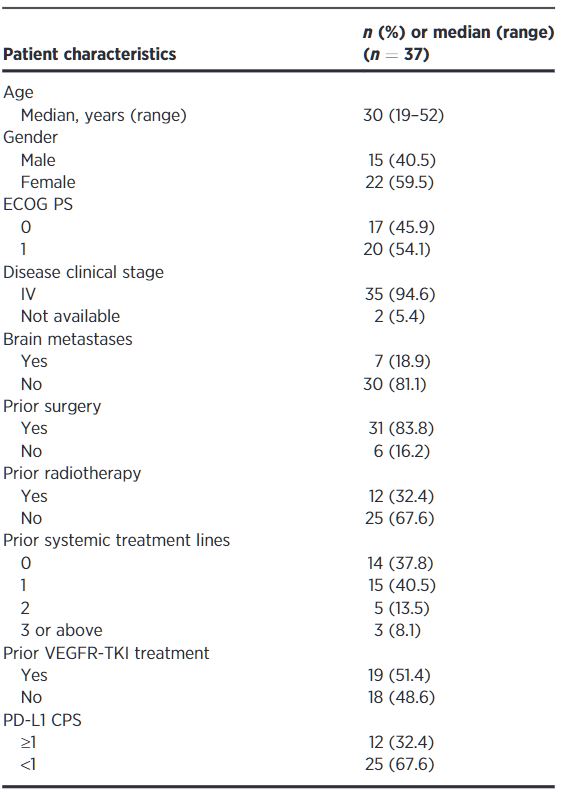
该研究是一项多中心、单臂的II期试验(Gxplore-005),在我国11个地点招募了18-75岁的、不可切除的、复发性或转移性ASPS患者,予以geptanolimab(3 mg/kg,静滴,1次/2周)治疗,直到病情进展或出现不可耐受的毒性。主要终点是客观缓解率。
2018年9月6日-2019年9月6日,共招募了37位患者接受geptanolimab治疗,其中23位(62.2%)既往接受过系统治疗。
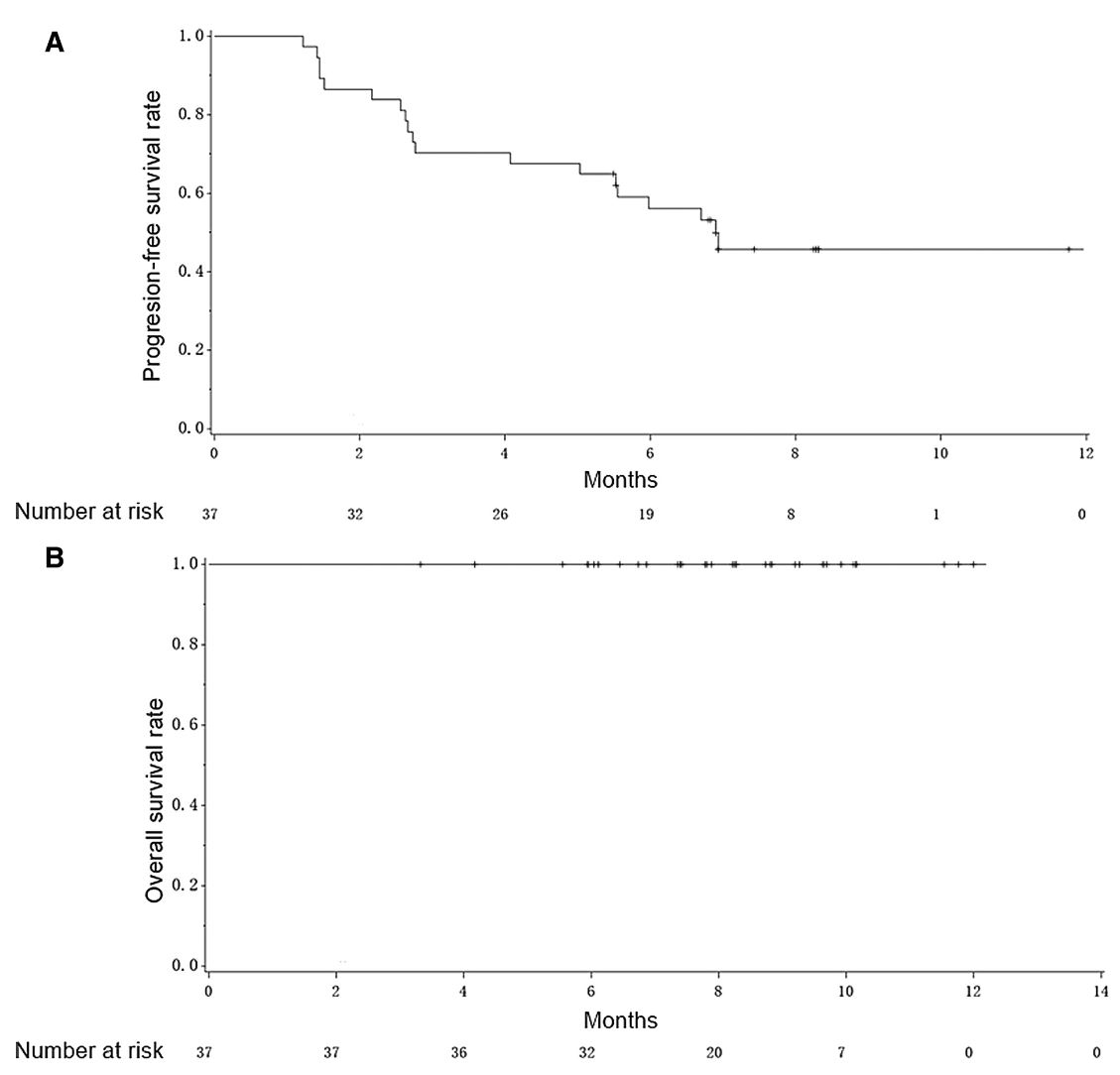
14位(37.8%)患者获得客观缓解,6个月持续缓解率达到91.7%。中位无进展存活期为6.9个月,32位(86.5%)患者获得病程控制。
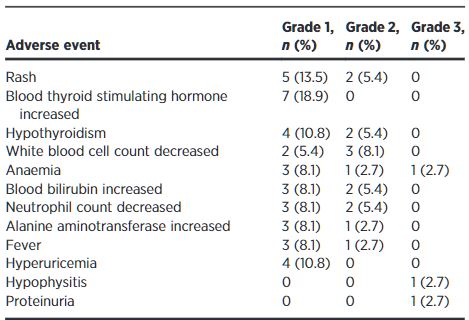
3位患者报告了3级治疗相关不良反应(TRAE),包括贫血、下垂体炎和蛋白尿(各一例[2.7%])。无4级TRAE。两位(5.4%)患者因TRAE终止治疗。CD4+T细胞的基础百分比与患者反应情况呈负相关。
综上所述,geptanolimab用于不可切除的复发性/转移性ASPS可获得具有临床意义的疗效,而且安全性可控。
原始出处:
Yuankai Shi, et al. Activity and Safety of Geptanolimab (GB226) for Patients with Unresectable, Recurrent, or Metastatic Alveolar Soft Part Sarcoma: A Phase II, Single-arm Study. Clin Cancer Res November 6 2020 DOI:10.1158/1078-0432.CCR-20-2819
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#肺泡软组织肉瘤#
59
#mAb#
54
#软组织#
66
#罕见#
54
#PD-1抗体#
72