JCO:北大肿瘤医院3期试验揭示多科室联合治疗转移性胃癌的临床获益
2021-01-12 Nebula MedSci原创
胃食管癌(EGC)是全球癌症相关死亡的第二大主要原因。当下,迫切需要有效的干预措施来改善转移性EGC患者的预后。本研究评估了早期跨学科支持治疗整合对转移性EGC患者的总体生存率(OS)的影响。
胃食管癌(EGC)是全球癌症相关死亡的第二大主要原因。当下,迫切需要有效的干预措施来改善转移性EGC患者的预后。本研究评估了早期跨学科支持治疗整合对转移性EGC患者的总体生存率(OS)的影响。
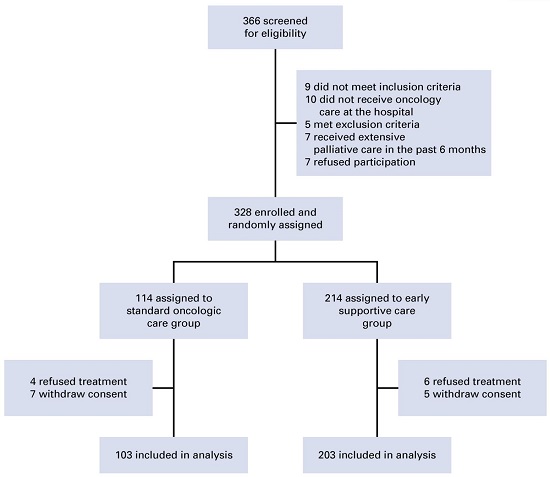
这是一项在北京大学肿瘤医院开展的开放性随机对照3期试验,招募了既往未治疗过的转移性EGC患者,按2:1随机分至早期跨学科支持治疗联合标准治疗(ESC)组或标准治疗(EC)组。ESC组患者接受由胃肠内科肿瘤专家、肿瘤护理专家、营养师和心理学家共同治疗;SC组患者接受仅标准的肿瘤治疗。主要终点是OS。
研究流程
2015年4月16日-2017年12月29日,共招募了328位患者:214位分至ESC组,114位分至SC组。截止2019年1月26日,有15位(5%)患者失访。
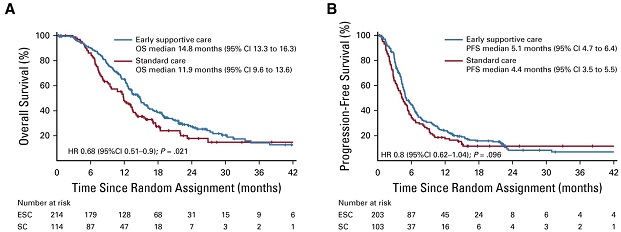
主要预后
ESC组的一线化疗的中位疗程为5个(IQR 4-7),SC组的为4个(IQR 2-6)。ESC组和SC组的中位OS分别是14.8个月(95% CI 13.3-16.3)和11.9个月(9.6-13.6;HR 0.68,95% CI 0.51-0.9;P=0.021)。
亚组预后
该研究表明,跨学科支持治疗的早期整合增加转移性胃癌患者的生存益处。未来值得进一步进行优化和标准化研究探索。
原始出处:
Zhihao Lu, et al. Early Interdisciplinary Supportive Care in Patients With Previously Untreated Metastatic Esophagogastric Cancer: A Phase III Randomized Controlled Trial. Journal of Clinical Oncology. January 07, 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#临床获益#
87
#JCO#
85
#转移性胃癌#
88
#肿瘤医院#
86
#联合治疗#
77
#转移性#
72
#3期试验#
85