Nature Medicine:全球万人晚期癌症测序成果发布,或开启癌症诊疗新模式
2017-05-15 佚名 奇点网
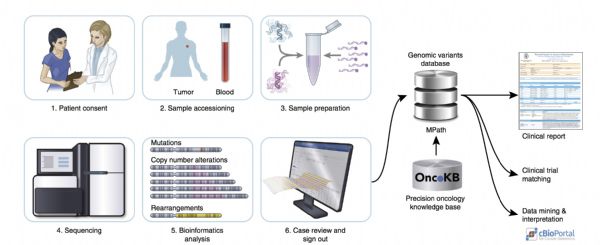
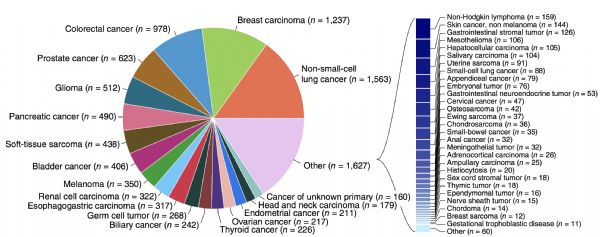
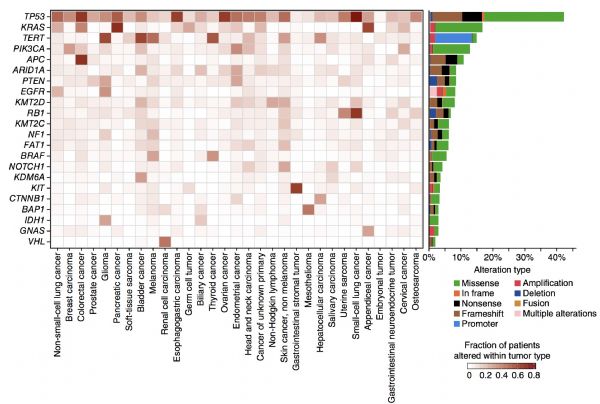
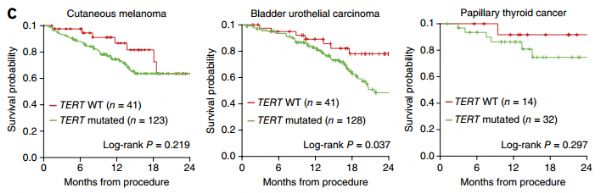
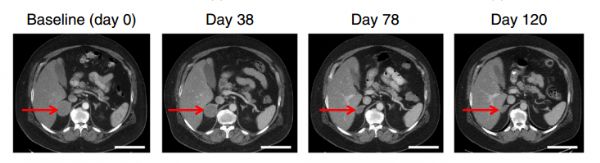
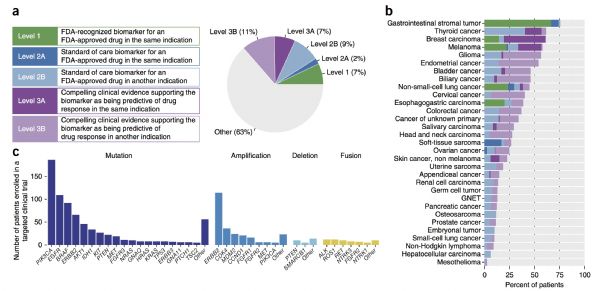
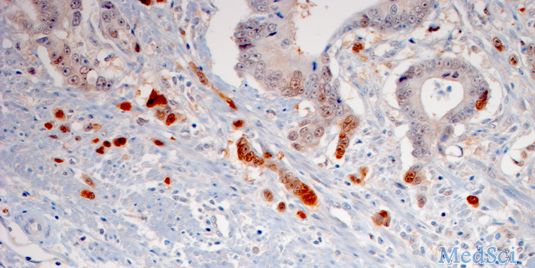
今天,《自然 医学》杂志上刊登了一个有关癌症的里程碑式临床研究[1]!美国最好的癌症中心之一,纪念斯隆凯特琳癌症研究中心(Memorial Sloan Kettering Cancer Center,简称MSK)的研究人员利用他们独有的肿瘤检测技术MSK-IMPACT对超过10000名晚期癌症患者进行了基因测序,这是目前转移性癌症患者中最大规模的肿瘤测序研究。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#DIC#
58
#Nat#
71
#CIN#
59
可以拿来直接临床使用?
71
#Medicine#
53
#Med#
53
学习了分享了
93
真是一个里程碑式的研究,有钱就是牛
86