Am J Cardiol: 经导管主动脉瓣置换的死亡率没有性别差异
2016-07-11 phylis 译 MedSci原创
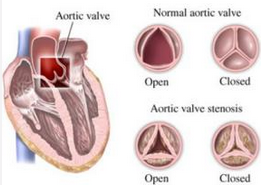
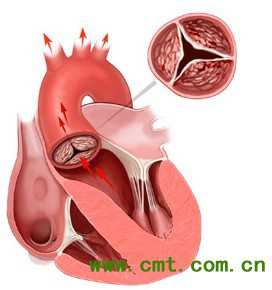
近年来由于经导管主动脉瓣置换(TAVR)的研究进展,重度主动脉瓣狭窄的治疗有了显著的改变。最近的CoreValve瓣膜研究表明,手术风险较高的患者,瓣膜主动脉瓣置换效果较好。但这种治疗的患者特征和预后的性别差异的研究较少。研究者比较应用CoreValve瓣膜行TAVR男性和女性的基线特征及临床预后。总共纳入3687例患者(1708名女性和1979名男性)。在基线水平,女性年纪稍大,比较脆弱,但她们
近年来由于经导管主动脉瓣置换(TAVR)的研究进展,重度主动脉瓣狭窄的治疗有了显著的改变。最近的CoreValve瓣膜研究表明,手术风险较高的患者,瓣膜主动脉瓣置换效果较好。但这种治疗的患者特征和预后的性别差异的研究较少。研究者比较应用CoreValve瓣膜行TAVR男性和女性的基线特征及临床预后。
总共纳入3687例患者(1708名女性和1979名男性)。在基线水平,女性年纪稍大,比较脆弱,但她们心脏疾病较少,左室收缩功能较好,冠状动脉疾病较少,卒中史较少。女性和男性的30天各种原因的死亡率分别为5.9%和5.8%,女性和男性1年的各种原因的死亡率分别为24.1%和21.3%。男性和女性30天卒中的发病率分别为5.7%和4%,1年的卒中发病率分别为9.3%和7.7%。女性比男性有较高的30天出血发生率,包括危及生命的出血和严重血管并发症的发生。女性和男性设备的成功率分别为86.9%和86.1%。
总之,尽管男性和女性应用CoreValve瓣膜行TAVR治疗基线和手术相关的并发症之间存在显著的差异,但并没有发现30天或1年死亡率存在显著差异。
原始出处:
Forrest JK, Adams DH, et al. Transcatheter Aortic Valve Replacement in Women Versus Men (from the US CoreValve Trials). Am J Cardiol. 2016 May 14.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Cardiol#
54
谢谢分享学习
66
#置换#
56
#主动脉瓣#
45
#主动脉#
40
#经导管#
62
#经导管主动脉瓣置换#
49