抗氧化治疗阿尔茨海默病“亮红灯”
2012-04-10 陈蓉 脉通编译
最近发表在 Archives of Neurology杂志的一篇研究表明,联合抗氧化治疗并不能改变阿尔茨海默病(AD)患者脑脊液中病理相关标志物水平[Arch Neurol. 2012 Mar 19.]。 研究显示在对轻中度AD患者使用维生素E、维生素C 和α硫辛酸(A
最近发表在 Archives of Neurology杂志的一篇研究表明,联合抗氧化治疗并不能改变阿尔茨海默病(AD)患者脑脊液中病理相关标志物水平[Arch Neurol. 2012 Mar 19.]。
研究显示在对轻中度AD患者使用维生素E、维生素C 和α硫辛酸(ALA)联合抗氧化治疗16周后,其淀粉样蛋白和tau蛋白相关的脑脊液标志物并没有改变,MMSE量表结果显示认知功能呈恶化趋势,但脑脊液中F2-isoprostane(脑内氧化应激水平的标志)水平显示轻度下降。研究同时显示大剂量辅酶Q10(CoQ)对于改善CSF标志物也没有任何益处。
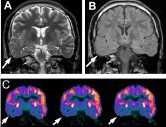
试验随机给予AD患者3种治疗中的1种:800IU/天维生素E+500mg/天维生素C+900mg/天ALA (E/C/ALA)或400 mgCoQ,一天三次或安慰剂治疗。治疗16周后发现与对照组相比,两个药物治疗组患者MMSE及ADCS-ADL分数均有下降。其中66例患者在治疗结束后检测了脑脊液中Aβ42,tau以及P-tau181蛋白的水平,表明联合抗氧化治疗并不影响淀粉样蛋白和tau蛋白病理相关的通路。
16-Week Changes in MMSE and ADCS-ADL by Group

研究者推测这种改变提示AD患者的认知功能下降有可能并不是由于AD相关病理标志物的恶化而致,关于其详细机制需要更长期的研究。同时研究者表示,尽管该实验为阴性结果,但有实际的临床意义,至少该研究在验证AD患者给予抗氧化药物治疗是否能够达到真正的预期效果方面是一个尝试。该研究结果不支持辅酶Q10作为进一步治疗AD药物的临床研究。
来源:Antioxidant Study in Alzheimer’s Raises Red Flag.Medscape Medical News,March 19,2012
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#阿尔茨海#
57
#阿尔茨#
82
#阿尔茨海默#
49