肝囊肿伴局部海绵状血管瘤变一例
2018-11-14 杜鹏 曹爱红 中国CT和MRI杂志
患者,女,62岁,主因发现肝脏占位一周入院。一周前体检时胸部CT发现肝右叶巨大囊实性占位,自诉无发热、纳差、腹痛、黄疸等症状,否认乙肝病史,无疫区接触史,实验室检查均正常。
1.一般资料
患者,女,62岁,主因发现肝脏占位一周入院。一周前体检时胸部CT发现肝右叶巨大囊实性占位,自诉无发热、纳差、腹痛、黄疸等症状,否认乙肝病史,无疫区接触史,实验室检查均正常。
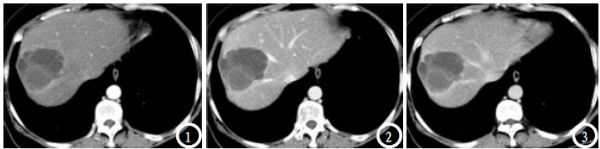
上腹部CT平扫+增强:肝右叶前上段不规则低密度影,内示分隔,病灶大小约7.0×6.1×5.7 cm,边界清晰,增强扫描病灶内分隔示轻度强化,囊性成分未示明显强化(图1-3)。诊断:肝右叶占位,感染性病变?
图1-3 肝右叶前上段不规则低密度影,内示分隔,边界清晰,增强扫描病灶内分隔示轻度强化,囊性成分未示明显强化。
MRI平扫+增强:肝右叶前上段囊实性混杂信号影,病灶内部分囊性病变呈短T1短T2信号影,未示明显强化(图4-6)。手术及病理:肝右叶第VIII段处可及一约6×7 cm大小肿瘤,肿瘤有包膜,部分突向肝膈面,部分呈囊性变,部分为实质性,实质部分质较硬,周边肝组织呈凹陷状纤维样变,肿瘤上方紧贴第二肝门,两侧后方紧贴肝中与肝右静脉,余肝及腹腔内未示明显肿瘤转移灶。病理诊断:(肝右叶)符合肝囊肿,局部区域示海绵状血管瘤表现,断面未见累及。
图4-6 肝右叶前上段囊实性混杂信号影,病灶内部分囊性病变呈短T1短T2信号影,未示明显强化。
2.讨论
囊肿和海绵状血管瘤均是肝内常见的良性病变,典型病变均具有特征性的影像学表现,但临床工作中常遇到影像表现不典型的病例,可能导致误诊和过度医疗。目前国内鲜有对于肝囊肿伴局部海绵状血管瘤变的报道,仅有杨昱曾报道肝囊肿伴囊肿壁血管瘤形成一例,其CT增强表现为病变部分呈典型血管瘤样强化,部分无强化,而本病例中,病灶内分隔示轻度强化,囊性成分始终未示明显强化。根据许一凯等对不典型肝血管瘤的强化表现分类,推测本病例中的局部海绵状血管瘤变符合第3种的强化方式,即病灶在各期的强化均不明显。
本病例为老年女性,根据患者的病史先除外肝包虫病的可能,但是其影像学表现又不能完全排除囊型肝棘球蚴病,同时,患者的影像学检查既不符合典型的肝囊肿,又与典型的肝海绵状血管瘤表现不同,且病灶体积较大,因此建议患者及家属施行外科手术治疗。
通过本病例的学习,进一步提醒我们,在临床工作中,不仅要熟悉病灶的典型影像学表现,对于一些少见的病例,要学会总结和分析,不断提高诊断水平, 为下一次的诊断工作打好基础。当然,影像诊断必须要结合临床和实验室检查,最终的确诊要依靠病理。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#囊肿#
63
#血管瘤#
62
#局部#
58
#海绵状血管瘤#
79
#海绵状#
68