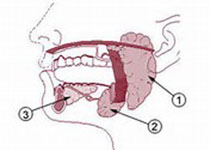
Oral Oncol:口腔癌的条件相对存活率调查
2017-09-14 MedSci MedSci原创
条件相对存活率(CRS)描述的是在诊断和治疗后已经存活一段时期的癌症患者的生存机会。因此,CRS可以完善那些未考虑患者诊断后存活时间的常规5年相对存活率。这篇研究的目的是为了评估韩国罹患口腔癌患者的5年CRS以及相关风险因素。
条件相对存活率(CRS)描述的是在诊断和治疗后已经存活一段时期的癌症患者的生存机会。因此,CRS可以完善那些未考虑患者诊断后存活时间的常规5年相对存活率。这篇研究的目的是为了评估韩国罹患口腔癌患者的5年CRS以及相关风险因素。研究在韩国肿瘤中心登记处筛选出1993-2013年间的15,329例诊断为口腔癌的患者病例。依据患者的性别、年龄、亚位点、组织学和诊断阶段计算CRS比率。结果显示,5年相对存活率为57.2%,而更进一步的分析显示,5年CRS在最初的2年间增加,并且在存活5年后上升至一定的平稳期,比率为86.5%。在存活5年后,女性的5年CRS要明显优于男性(90.0% vs. 83.3%),并且≤45岁患者的5年CRS要优于年长患者(93.3% vs. 86.4%或86.7%)。另外,5年CRS存在亚位点特异性的差异(舌: 91% vs. 口底: 73.9%)。鳞状细胞癌的CRS为87.3%,其他组织分型为85.5%。局限性疾病的CRS为95.7%,有部位转移的为87.3%。结论:依据患者的性别、年龄、亚位点、组织学和诊断阶段的不同,口腔癌患者呈现出上调的CRS比率。因此,在最初
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#存活率#
53
#Oral#
69
#Oncol#
55
学习了很有用不错
98
学习了谢谢分享
89
学习了.涨知识
102
不错的.学习了.谢谢分享!
104