Cancer Cell:鉴定出混合性白血病的新药物靶标
2012-04-10 towersimper 生物谷
混合性白血病(mixed lineage leukaemia, MLL)是一种具有侵袭性的急性骨髓性白血病(acute myeloid leukaemia)。 来自英国曼彻斯特大学帕特森癌症研究所(Paterson Institute for Cancer Research)的一个研究小组鉴定出混合性白血病(MLL)的一种新的药物靶标,即酶LSD1。LSD1有助于控制某些致癌基因是被关闭还是被开

混合性白血病(mixed lineage leukaemia, MLL)是一种具有侵袭性的急性骨髓性白血病(acute myeloid leukaemia)。
来自英国曼彻斯特大学帕特森癌症研究所(Paterson Institute for Cancer Research)的一个研究小组鉴定出混合性白血病(MLL)的一种新的药物靶标,即酶LSD1。LSD1有助于控制某些致癌基因是被关闭还是被开启,而且是维持白血病干细胞潜能的一种关键性的调节物。阻断这种酶就可阻止促进癌症产生的蛋白表达。
来自英国癌症研究协会帕特森药物开发中心(Cancer Research UK’s Paterson Drug Discovery Unit)的科学家们合成出阻断LSD1的分子。论文通信作者和英国癌症研究协会白血病生物学实验室小组负责人Tim Somervaille博士证实这些分子能够阻止从患有混合性白血病(MLL)病人身上提取的白血病细胞生长,同时也阻止来自患有MLL疾病的小鼠的白血病细胞生长。
急性骨髓性白血病病人存活率一直比较低。患有混合性白血病的病人很难用当前的治疗方法,如密集化疗(intensive chemotherapy)和骨髓移植,获得治愈,而且他们目前还不能获得针对性药物来治疗,因而他们迫切需要新的药物。
在当前研究中,尽管研究人员还需开展更多研究来进一步测试这些分子,但是这些发现已经为人们在未来开发出新的治疗方法打下坚实的基础。(生物谷:towersimper编译)

doi:10.1016/j.ccr.2012.03.014
PMC:
PMID:
The Histone Demethylase KDM1A Sustains the Oncogenic Potential of MLL-AF9 Leukemia Stem Cells
William J. Harris1, Xu Huang1, James T. Lynch1, Gary J. Spencer1, James R. Hitchin2, Yaoyong Li3, Filippo Ciceri1, Julian G. Blaser1, Brigit F. Greystoke1, Allan M. Jordan2, Crispin J. Miller3, Donald J. Ogilvie2, Tim C.P. Somervaille
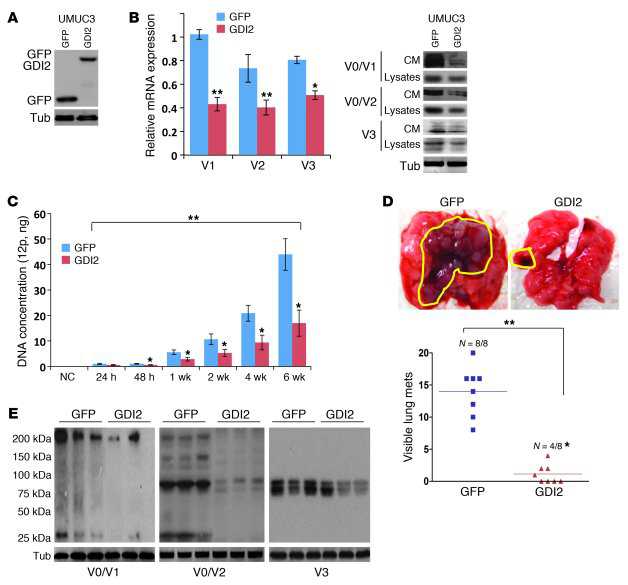
Using a mouse model of human MLL-AF9 leukemia, we identified the lysine-specific demethylase KDM1A (LSD1 or AOF2) as an essential regulator of leukemia stem cell (LSC) potential. KDM1A acts at genomic loci bound by MLL-AF9 to sustain expression of the associated oncogenic program, thus preventing differentiation and apoptosis. In vitro and in vivo pharmacologic targeting of KDM1A using tranylcypromine analogs active in the nanomolar range phenocopied Kdm1a knockdown in both murine and primary human AML cells exhibiting MLL translocations. By contrast, the clonogenic and repopulating potential of normal hematopoietic stem and progenitor cells was spared. Our data establish KDM1A as a key effector of the differentiation block in MLL leukemia, which may be selectively targeted to therapeutic effect.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新药物#
84
#CEL#
0
#Cell#
71
#cancer cell#
70
#靶标#
59
#药物靶标#
66