BMJ:垂体瘤卒中——案例报道
2016-02-18 Mechront 译 MedSci原创
患者男,85岁,因“头痛、呕吐、双眼进行性视力丧失5天”就诊。否认体重下降、惊厥、肢体或面部不适等。有高血压、腹主动脉瘤、甲状腺功能减退和良性前列腺肥大。血压110/75 mm Hg,心律齐 80次/分,格拉斯哥昏迷评分 (GCS) 15。周围神经系统检查未见明显异常。颅神经检查提示双颞侧偏盲,眼底检查未见明显异常。钠 126 mmol/L(参考范围135-145),钾 3.6 mmol/L (3
患者男,85岁,因“头痛、呕吐、双眼进行性视力丧失5天”就诊。
否认体重下降、惊厥、肢体或面部不适等。有高血压、腹主动脉瘤、甲状腺功能减退和良性前列腺肥大。
血压110/75 mm Hg,心律齐 80次/分,格拉斯哥昏迷评分 (GCS) 15。周围神经系统检查未见明显异常。颅神经检查提示双颞侧偏盲,眼底检查未见明显异常。
钠 126 mmol/L(参考范围135-145),钾 3.6 mmol/L (3.5-5),尿素 5.6 mmol/L (2.5-6.7),肌酐 101 µmol/L (70-150),C反应蛋白(CRP) 66 mg/L (<10)。全血细胞计数和肝功能是正常的。
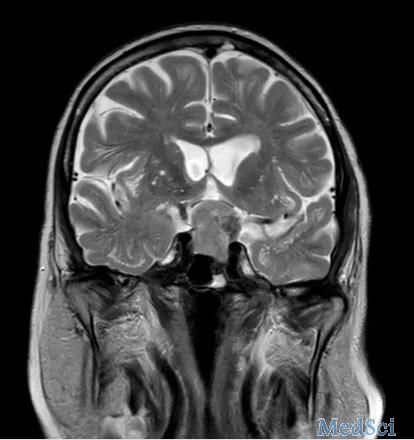
CT:垂体窝有个肿块。MRI:鞍区肿块压迫视交叉,信号变化提示肿块内出血。如下图:
患者表现为双颞侧偏盲,需要考虑的诊断有:垂体腺瘤、垂体卒中、颅咽管瘤、脑膜瘤、胶质瘤、颅内动脉瘤。
结合患者临床表现和辅助检查,垂体瘤卒中的可能性最大。垂体瘤卒中指预先存在的垂体肿瘤发生出血或梗塞,垂体腺瘤发生卒中的风险为2-7%。垂体腺瘤比微腺瘤患者发生卒中的风险更大。
脑垂体位于刚性壁内,快速增长导致鞍内压力增高,以致于出现一系列临床表现:头痛(可以伴有恶心、呕吐);正常血管受压,导致垂体功能低下,垂体前叶促肾上腺皮质激素分泌受损,进而导致皮质醇不足;视交叉受压,导致视野缺损和视力下降;海绵窦内结构受压,导致颅神经麻痹。
垂体卒中患者出现日益恶化的体重或GCS减小,均是外科急诊切除肿瘤的指征;病情稳定的患者可以选择保守治疗,但如果不改善,可能需要进行手术治疗。
所有垂体卒中患者应该在首次发病后的4-8周进行随访;每年要去内分泌科随访;发病后3-6个月进行头颅MRI检查,此后每年行一次头颅MRI检查连续5年,然后每2年进行一次头颅MRI检查。
本例中的患者成功的接受了内镜下经蝶切除垂体瘤,激素水平恢复到正常,右眼视力得到改善,但是左眼视力恢复差。
原始出处:
Ramdeep Bajwa, Paven Preet Kaur, Headaches and hormones: a potentially lethal combination.BMJ 2016; 352 doi: http://dx.doi.org/10.1136/bmj.h6752
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BMJ#
65
还是少见
148
最终还是靠MRI
141
不错的文章
165
#垂体瘤#
75
#垂体#
64