盘点:2016胰岛素抵抗研究重要进展一览
2016-09-14 MedSci MedSci原创
胰岛素抵抗是一种“沉默”的危险因素,与糖尿病和心血管疾病的其他危险因素并存,当它不再沉默而是导致2型糖尿病患者血糖水平升高时,胰岛素抵抗仍然存在。糖尿病前期或糖尿病未发展前胰岛素抵抗本身并不存在任何迹象或症状,仅存在胰岛素抵抗时机体的血糖水平也可以是正常的。而肥胖或超重,存在高血压或糖尿病家族史的人群,胰岛素抵抗则变成了糖尿病和心血管疾病的一个危险因素。这里小M整理了2016年以来关于胰岛素抵
胰岛素抵抗是一种“沉默”的危险因素,与糖尿病和心血管疾病的其他危险因素并存,当它不再沉默而是导致2型糖尿病患者血糖水平升高时,胰岛素抵抗仍然存在。糖尿病前期或糖尿病未发展前胰岛素抵抗本身并不存在任何迹象或症状,仅存在胰岛素抵抗时机体的血糖水平也可以是正常的。而肥胖或超重,存在高血压或糖尿病家族史的人群,胰岛素抵抗则变成了糖尿病和心血管疾病的一个危险因素。这里小M整理了2016年以来关于胰岛素抵抗的重要研究与大家分享。
【1】 非糖尿病的绝经后女性,胰岛素抵抗可影响骨的结构
欧登塞大学医院内分泌科的Vikram V. Shanbhogue博士和同事对146名绝经后妇女(平均年龄60.3岁)进行了研究,所有女性均没有糖尿病,研究者试图探究胰岛素抵抗对周围骨几何结构、体积骨密度、骨微结构和估计的骨强度的影响。结果表明,对于非糖尿病的绝经后妇女,外周胰岛素抵抗和高胰岛素血症的存在对骨密度和骨微结构有益,表明在外周胰岛素抵抗的条件下,骨细胞可能仍然对胰岛素的活动是敏感的。
研究中发现,与低HOMA-IR组相比,高HOMA-IR组在全髋、腰椎有更大面积的骨密度;在桡骨、胫骨有更高比例的皮质/总骨面积;在桡骨和胫骨有更高总体积BMD;在桡骨和胫骨有更高皮质厚度;在胫骨有更低的皮质骨松化,在桡骨有更多的骨小梁数量;以及在桡骨和胫骨有更大的骨小梁厚度;此外,还有更大的估计骨刚度。(文章详见——J Clin Endocrinol Metab:非糖尿病的绝经后女性,胰岛素抵抗和骨结构研究)
【2】 JCEM:青少年脂肪组织胰岛素抵抗与游离脂肪酸有关
近期发表在J Clin Endocrinol Metab的研究称,口服葡萄糖耐量试验(OGTT)中,脂肪组织胰岛素抵抗与游离脂肪酸抑制的下降有关。
研究人员对962名肥胖青少年进行了研究,通过葡萄糖耐量评估脂肪组织胰岛素抵抗情况,以及OGTT过程中,脂肪组织胰岛素抵抗与游离脂肪酸的关系。基于糖耐量情况参与者被分为3组:正常糖耐量组(n = 770)、前驱糖尿病组(n = 170)和糖尿病组(n = 22)。
数据显示,不同糖耐量区间内,脂肪胰岛素抵抗明显增加。与青春期的参与者相比,青春期前的儿童有较高的空腹游离脂肪酸和较低的空腹胰岛素和较低的脂肪组织胰岛素抵抗指数。
接着研究者对115名参与者进行了腹部MRI检测脂质分配,研究者发现脂肪组织胰岛素抵抗指数与内脏脂肪密切相关,与内脏/腹部脂肪比也密切相关,不过与腹部皮下脂肪无关。
不同糖耐量区间内,游离脂肪酸的曲线下面积(AUC)显著降低;糖耐量正常组游离脂肪酸抑制程度更大。AUC游离脂肪酸和脂肪组织胰岛素抵抗指数显著相关。糖耐量范围、BMI Z评分、IL-6和脂联素可作为脂肪组织胰岛素抵抗的预测因子。(文章详见——JCEM:青少年脂肪组织胰岛素抵抗与游离脂肪酸有关)
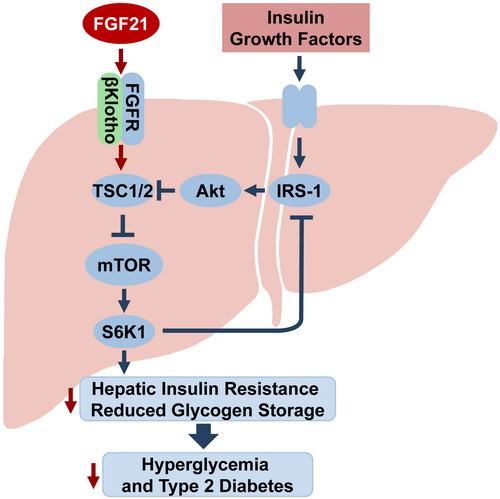
【3】 FGF21改善胰岛素抵抗作用机制被揭示
国际学术期刊Hepatology在线发表了中国科学院上海生命科学研究院营养科学研究所李于研究组的最新研究成果揭示了成纤维细胞生长因子21(FGF21)作为营养感受器mTORC1复合物的抑制剂,以自分泌或旁分泌的方式调控肝脏的胰岛素敏感性和全身葡萄糖代谢平衡。
研究人员龚琦等在该实验室前期研究基础上,通过深入的体内和体外小鼠实验发现,当敲低FGF21的肝脏特异性受体βKlotho后,FGF21的胰岛素增敏作用和降血糖效应会降低;在小鼠肝脏、原代肝细胞和人的肝脏细胞系中,FGF21能抑制由胰岛素抵抗引起的mTORC1活性的增加,证明FGF21是mTORC1的一个负性调节因子;实验还发现,当过表达mTORC1的下游关键分子S6K1后,FGF21对小鼠肝脏和原代肝脏细胞的胰岛素增敏作用消失,进一步研究表明,FGF21是通过激活肝脏和原代肝细胞中胰岛素信号通路,进而促进糖原合成,基因敲除TSC1会激活mTORC1,从而抑制FGF21对肝原代细胞糖原合成能力的促进作用,由此推测,FGF21可能是通过抑制mTORC1来促进肝糖原的合成。
该研究揭示了FGF21在改善肝脏胰岛素敏感性和葡萄糖代谢平衡时,直接作用于肝脏,FGF21可能作为mTORC1复合体的抑制因子,通过抑制mTORC1复合体的活性,增加肝脏胰岛素敏感性,促进肝脏糖原储存来增加葡萄糖的利用,从而调节全身葡萄糖代谢的动态平衡。(文章详见——Hepatology:FGF21改善胰岛素抵抗作用机制被揭示)
【4】 补充维生素D可避免早发型胰岛素抵抗
近期发表在Diabetes, Obesity and Metabolism杂志的研究称,对维生素D不足的患者早期使用维生素D进行干预,可以避免早发型胰岛素抵抗。
来自色列贝尔谢巴本班古里昂大学的Sigal Tepper博士和同事对130名没有糖尿病的男性进行了一项研究,参与者平均年龄47.25岁,血清25(OH)D<20 ng/mL。将参与者分为补充维生素D治疗组(维生素D 100,000 IU,每月两次)和对照组。
研究人员发现,校正基线维生素D水平、年龄、BMI、阳光暴露、运动和低密度脂蛋白等混杂因素后,两组间在胰岛素和自稳态模型评估胰岛素抵抗(HOMA-IR)方面存在差异。补充维生素D的治疗组参与者,其胰岛素和HOMA-IR水平稳定,但是对照组的增加了16%。(文章详见——Diabetes Obes Metab:补充维生素D可避免早发型胰岛素抵抗)
【5】 脂肪组织中ALA含量与胰岛素抵抗呈负相关
有研究表明,n-3 (ω-3)脂肪酸(FAs) 对心血管代谢危险因素有益,但是脂肪组织α-亚麻酸(ALA)、二十碳五烯酸(EPA)和二十二碳六烯酸(DHA)与胰岛素抵抗间的联系仍未知。因此研究者对健康成年人进行了一项横断面研究,使用多因素分析探究脂肪组织n-3 FAs (总n-3 FAs、ALA、EPA+DHA)与胰岛素抵抗间的联系。AHS-2队列中所有成年参与者(716人,平均年龄58岁)。结果显示,成年男女性脂肪组织中更高含量的ALA与胰岛素抵抗呈负相关,尤其是腰围在正常范围的个体。
研究数据显示,与最低三分之一组相比,脂肪组织ALA最高组与HOMA-IR呈负相关。通过腰围进行分层分析后,女性腰围≤88 cm组或男性腰围≤102 cm组中,ALA仍与HOMA-IR呈负相关;但是在更大腰围组,没有发现这种关系。研究者也没有观察到脂肪组织EPA+DHA与HOMA-IR间的关系。(文章详见——Am J Clin Nutr:脂肪组织中ALA含量与胰岛素抵抗呈负相关)
【6】 一文彻底了解胰岛素抵抗
来自糖尿病、心脏病和公共卫生医学领域的人员认为最近几年关于胰岛素抵抗的科学研究取得了一些进展。直到本世纪,胰岛素抵抗和糖尿病前期才开始受到医学研究的重点关注。
胰岛素抵抗综合征,代谢综合征,甚至是X综合征,这些术语指的是与胰岛素抵抗相关的危险因素群。
相比之下,自17世纪以来糖尿病的经典症状:多尿和口渴,早已被大众所了解。一个多世纪前,研究人员又发现了胰腺和胰岛素在糖尿病中的作用。
目前已将胰岛素抵抗作为2型糖尿病的发病因素,但是2型糖尿病的病因并没有这么简单。那么胰岛素抵抗到底是什么,它又是如何发展而来的?这篇文章从多个方面详细介绍了胰岛素抵抗,相信看了这篇文章大家一定会对胰岛素抵抗有更深的理解。(文章详见——一篇文章让你彻底了解胰岛素抵抗)
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#重要进展#
59
#胰岛#
67
谢谢指点谢谢
98
文章很好,非常有益
90
学习了,长知识
87
学习学习。。
79
学习了,赞一个!!!
118
整理的很好,系统学习了,感谢分享
58
这篇要收藏
56
学习了,赞一个!
55