cell rep:科学家发现靶向癌症治疗的新方法
2017-09-27 佚名 Medicalxpress
针对个体患者的需求定制独特的化疗方法的精密医学在今天的癌症治疗中变得越来越重要了。近来,科学家们发现了分子生物诊断可以精确地识别肿瘤细胞的变化。众所周知,现代癌症治疗的主要目的是开发单独靶向这些改变了的肿瘤细胞但是却不会影响周围健康的细胞的新药物。
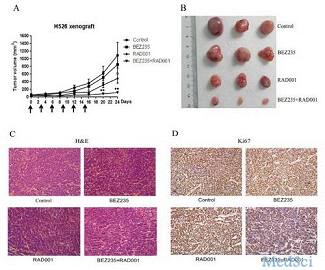
科罗拉多教授和罗马托马斯教授的工作组以及科罗拉多大学医院病理学系和翻译基因组系的Martin Sos教授已经测试了1500多种不同的物质对不同种类的癌细胞的影响。这项测试程序是与多特蒙德技术大学,多特蒙德领先发现中心等国际集团合作进行的。
原始出处:
Johannes Brgelmann,Marcel A.Dammert,FelixDietlein et al, Systematic Kinase Inhibitor Profiling Identifies CDK9 as a Synthetic Lethal Target in NUT Midline Carcinoma, Cell Reports (2017). DOI: 10.1016/j.celrep.2017.08.082 Volume 20, Issue 12, 19 September 2017, Pages 2833-2845
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CEL#
47
#科学家发现#
59
#癌症治疗#
55
#Cell#
69
#新方法#
45
文章很好!值得分享!
102