STM:结肠癌药物治疗的新选择
2015-04-04 Zhang JL译 MedSci原创
来自新加坡南洋理工大学(NTU Singapore)和欧洲最大的医科大学——瑞典卡罗林斯卡医学院的研究人员发现,现有用于治疗白血病的化疗药物可以预防和控制结直肠肿瘤的生长。大肠癌是常见的恶性肿瘤,包括结肠癌和直肠癌。大肠癌的发病率从高到低依次为直肠、乙状结肠、盲肠、升结肠、降结肠及横结肠,近年有向近端(右半结肠)发展的趋势。其发病与生活方式、遗传、大肠腺瘤等关系密切。发病年龄趋老年化,男女之比为1
来自新加坡南洋理工大学(NTU Singapore)和欧洲最大的医科大学——瑞典卡罗林斯卡医学院的研究人员发现,现有用于治疗白血病的化疗药物可以预防和控制结直肠肿瘤的生长。
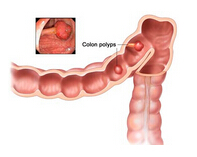
大肠癌是常见的恶性肿瘤,包括结肠癌和直肠癌。大肠癌的发病率从高到低依次为直肠、乙状结肠、盲肠、升结肠、降结肠及横结肠,近年有向近端(右半结肠)发展的趋势。其发病与生活方式、遗传、大肠腺瘤等关系密切。发病年龄趋老年化,男女之比为1.65:1。结直肠癌是世界范围内三个最常见的癌症之一,而在新加坡则是最常见的肿瘤。几乎95%的结直肠肿瘤是恶性肿瘤。
伊马替尼(Imatinib)是一种用于治疗费城染色体(Bcr-Abl)阳性的慢性骨髓性白血病(简称CML)成人患者的急变期、加速期和干扰素治疗失败后的慢性期的口服药物。既往研究也证明伊马替尼对胃肠道间质瘤治疗也有效,有效率在50%左右。本研究人员发现,伊马替尼是通过阻断信号通路相关的一组称为EphB的细胞受体而发挥作用的。这意味着当用于治疗患有结肠肿瘤的老鼠,它能够将肠道内肿瘤的生长速度减半。
对于原发病灶已经过手术切除后发生复发的患者来说,这一研究发现为目前无有效药物治疗的灰霾带来希望的曙光。这项研究结果发表在最新一期Science Translational Medicine杂志上。
卡罗林斯卡医学院Pettersson 教授称:“我们的发现具有重要的临床意义,因为对于进展期结直肠癌患者来说,伊马替尼是一种潜在有效的新药物治疗,它能够抑制肿瘤形成并延缓肿瘤进展。”
该研究的第一作者、Pettersson 教授实验室的高级研究员Parag Kundu博士指出,在他们的测试中,伊马替尼能够在干细胞水平阻止肿瘤形成,并且显著降低肿瘤生长和扩散速度。此外,在取自人类患者的结肠肿瘤组织中应用伊马替尼进行测试收到了相同的效果。
结肠癌通常发展首先是从良性肿瘤开始,当没有及时治疗时发生恶性转化,并可能扩散到身体的其他部位。对于结肠癌早期阶段的主要治疗是通过手术对受影响的肠段进行切除。
科学家们说这些发现还表明短期内间歇化疗可能作为优化的治疗模式,因为这将大大减少长期使用伊马替尼时所产生的副作用。
原始出处:
P. Kundu, M. Genander, K. Straat, J. Classon, R. A. Ridgway, E. H. Tan, J. Bjork, A. Martling, J. van Es, O. J. Sansom, H. Clevers, S. Pettersson, J. Frisen. An EphB-Abl signaling pathway is associated with intestinal tumor initiation and growth. Science Translational Medicine, 2015; 7 (281): 281ra44 DOI:10.1126/scitranslmed.3010567
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#STM#
66
不错,学习了
124
需继续研究…
127
真心不错
129
了解……
94
嗯
151
嗯
102
真的可以吗
115
支持下
125