Sci. Transl. Med.:肽类分子E4带来抗纤维化新希望
2012-06-17 bo 生物谷
5月30日,Sci. Transl. Med.杂志报道,科学家发现一种新的肽类分子E4,可发挥抗器官纤维化功效。纤维增殖异常如先天性肺纤维化和系统性硬化,由于没有有效的治疗手段,常导致进展性器官纤维化进而引发显著的致病和致死率。 为解决这一突出问题,研究者在人类及小鼠模型,体内及体外多个实验条件下,检测了来源于内皮他汀的肽类对已有纤维化以及TGF-β和争光霉素诱发纤维化的效果。 研究发现了,一
5月30日,Sci. Transl. Med.杂志报道,科学家发现一种新的肽类分子E4,可发挥抗器官纤维化功效。纤维增殖异常如先天性肺纤维化和系统性硬化,由于没有有效的治疗手段,常导致进展性器官纤维化进而引发显著的致病和致死率。
为解决这一突出问题,研究者在人类及小鼠模型,体内及体外多个实验条件下,检测了来源于内皮他汀的肽类对已有纤维化以及TGF-β和争光霉素诱发纤维化的效果。
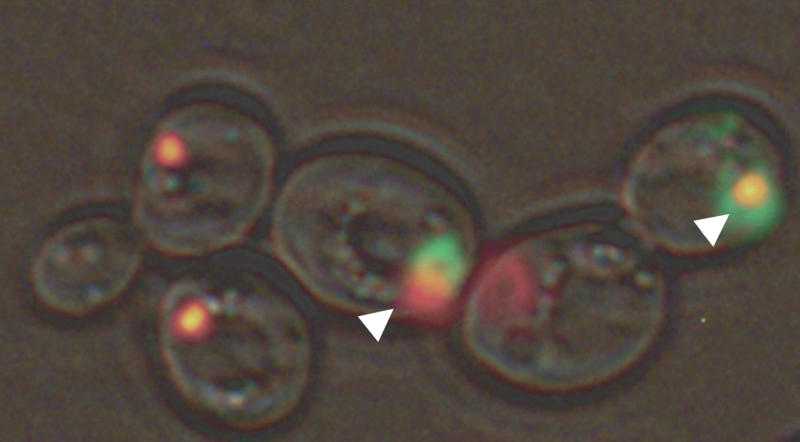
研究发现了,一种叫E4的肽具有强烈的抗纤维化活性。E4可在多个实验条件下防止TGF-β诱发的皮肤纤维化:如小鼠模型体内实验;人类皮肤体外实验;争光霉素诱导的皮肤和肺纤维化体内实验。
此外,E4在上述模型中显著降低已有的纤维化。E4介导的纤维化改善伴有细胞凋亡的减少,催化胶原交联的赖氨酰氧化酶的水平降低,以及促进纤维化的转录因子Egr-1的减少。
总之,他们的发现证实,E4具有显著的抗纤维化活力,并可能作为治疗器官纤维化的因子。

doi:10.1016/j.cell.2011.10.017
PMC:
PMID:
A Peptide Derived from Endostatin Ameliorates Organ Fibrosis
Yukie Yamaguchi1, Takahisa Takihara1, Roger A. Chambers1, Kristen L. Veraldi1, Adriana T. Larregina2 and Carol A. Feghali-Bostwick1,*
Fibroproliferative disorders such as idiopathic pulmonary fibrosis and systemic sclerosis have no effective therapies and result in significant morbidity and mortality due to progressive organ fibrosis. We examined the effect of peptides derived from endostatin on existing fibrosis and fibrosis triggered by two potent mediators, transforming growth factor–β (TGF-β) and bleomycin, in human and mouse tissues in vitro, ex vivo, and in vivo. We identified one peptide, E4, with potent antifibrotic activity. E4 prevented TGF-β–induced dermal fibrosis in vivo in a mouse model, ex vivo in human skin, and in bleomycin-induced dermal and pulmonary fibrosis in vivo, demonstrating that E4 exerts potent antifibrotic effects. In addition, E4 significantly reduced existing fibrosis in these preclinical models. E4 amelioration of fibrosis was accompanied by reduced cell apoptosis and lower levels of lysyl oxidase, an enzyme that cross-links collagen, and Egr-1 (early growth response gene–1), a transcription factor that mediates the effects of several fibrotic triggers. Our findings identify E4 as a peptide with potent antifibrotic activity and a possible therapeutic agent for organ fibrosis.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Transl#
93
#新希望#
63
#Transl.#
66
#TRA#
76
#抗纤维化#
79
#Med#
57