Lancet Gastroenterology& Hepatology:CT结直肠检查后成像后结直肠癌或间隔癌发病率
2018-02-20 MedSci MedSci原创
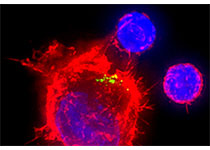
CT结肠镜检查对结直肠癌高度敏感,但间隔期或成像后的结直肠癌患病率(CT结肠镜检查时阴性后确诊癌症)像其潜在原因一样尚且未知。近日,Lancet子刊上发表一篇文献,对CT结肠镜检查成像后结直肠癌的发病率和病因进行系统回顾和meta分析。研究人员对MEDLINE、Embase和Cochrane中心注册的对照试验进行系统检索。筛选1994年1月1日-2017年2月28日期间发表的根据国际通识标准行CT
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Gastroenterol#
57
#发病率#
67
#Lancet#
60
#癌发病#
63
#GAS#
64
#AST#
57
学习了.谢谢作者分享!
103
#癌发病率#
81
打字员.学习了.
96
学习了.谢谢分享.
85