J Clin Oncol:儿童低级别胶质瘤中BRAF V600E突变对治疗和预后的意义
2017-07-26 王强 肿瘤资讯
儿童低级别胶质瘤中,BRAF V600E的生物学意义和临床意义尚未完全明确。本文即对这一问题进行了研究。
儿童低级别胶质瘤(pediatric low-grade gliomas,PLGG)是儿童最常见的脑肿瘤,其部位、组织学类型、发病年龄、临床生物学行为方面均有一定异质性。随着遗传学研究的深入,目前已认识到某些PLGG会有涉及RAS/MAPK通路活化的遗传学改变,但其他通路的突变相对较少,加之这类改变对治疗和临床预后的意义尚未明确,因此目前PLGG的非手术治疗并未涉及肿瘤的分子生物学改变。
BRAF V600E突变就是这样一个例子:部分成人和儿童肿瘤中可见该突变,但PLGG中仅有少数具有该突变。具有BRAF V600E突变的PLGG在自然病程和预后方面是否有自身特点,也还有争议。有鉴于此,加拿大多伦多大学Hawkins和Tabori教授在前期研究基础上对南安大略地区诊断和治疗的一组PLGG患者进行了临床和遗传学方面的研究,相关文章提前在线发表于美国临床肿瘤学会(ASCO)官方杂志Journal of Clinical Oncology,肿瘤资讯为大家编译介绍如下。
相关临床数据来自南安大略地区儿童医院(SickKids)1985年1月至2015年12月间诊断和治疗的所有PLGG患者;从病理角度,该研究中的PLGG指的是胶质瘤、混合性神经元-胶质肿瘤,均为第四版WHO中枢神经系统肿瘤分类归为I级、II级的肿瘤;除外室管膜瘤、伴间变的多形性黄色瘤型星形细胞瘤、室管膜下巨细胞型星形细胞瘤。总计510例可供组织学和BRAF V600E分析并进行预后和疗效分析;其中2000-2015年间确诊的449例可进行部位及病理学亚型与BRAF V600E突变关系的分析,405例具有分子遗传学数据可供分析。另外,联合18个国际性儿科中心进行了BRAF V600E突变PLGG预后分析。具体结果如下:
SickKids 2000-2015年间治疗的405例PLGG患者中,69例(17%)具有BRAF V600E突变;BRAF V600E突变肿瘤可见于所有年龄、中枢神经系统的所有部位,但更常见于中线部位,如视觉通路、脑干、脊髓,33%的BRAF V600E突变PLGG发生自中线部位(间脑及脑干)。大部分PLGG病理学亚型中均可见BRAF V600E突变,但部分亚型中更多见,本研究中多见该突变的病理类型依次为多形性黄色瘤型星形细胞瘤(78%)、神经节细胞胶质瘤(49%);弥漫性星形细胞瘤(43%)及WHO I级的星形细胞瘤(20%)也常见该突变。
对510例PLGG患者的长期生存数据(随访时间0.01年-28年,平均7年)分析表明,具有BRAF V600E突变者(n=99)会持续进展、未能达到平台期。5年、10年的无进展生存及总生存数据详见表1A、B。BRAF V600E突变PLGG患者甚至在随访25年时出现了肿瘤进展导致的死亡。生存分析表明BRAF V600E突变者的预后显着差于BRAF KIAA1549融合者(图1C、D)。
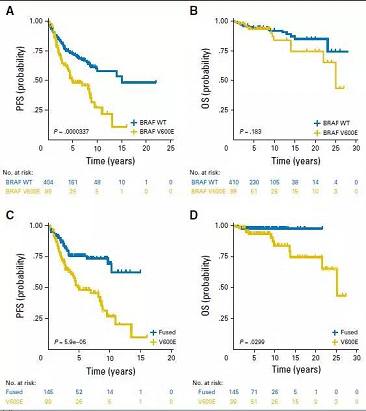
图1. SickKids数据中根据BRAF V600E状态进行分层的患者生存情况。(A)BRAF V600E是否突变时的无进展生存;(B)BRAF V600E是否突变时的总生存;(C)BRAF V600E突变与KIAA1549融合的无进展生存;(D)BRAF V600E突变与KIAA1549融合的总生存。WT为野生型
SickKids患者中44.4%达到了手术完全切除,但BRAF V600E突变PLGG患者中很多切除后仍出现了进展。完整切除与未能完整切除者的5年无进展生存分别为67.8%、38.8%,BRAF野生型患者完整切除与未能完整切除者的5年无进展生存分别为95.9%、53.3%;而BRAF V600E突变者放、化疗后的预后也较差:放疗后的5年、10年无进展生存分别为42.2%、28.1%。BRAF V600E突变者有32%进行了化疗,一线化疗后的5年无进展生存为30.4%。
SickKids数据中有403例PLGG可进行CDKN2A拷贝数分析。BRAF V600E突变PLGG患者中25%存在CDKN2A缺失,而野生型PLGG中这一数据为17%。CDKN2A缺失者生存和无进展生存均较差,但这一作用仅限于BRAF V600E突变者。BRAF V600E突变PLGG患儿中,CDKN2A缺失与平衡者的5年无进展生存分别为24.0%、68.7%,10年无进展生存分为0%、45.9%。
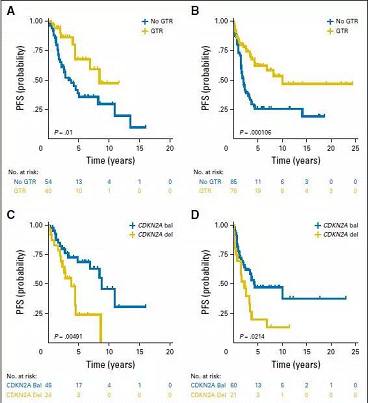
图2. SickKids数据中根据手术切除范围及BRAF CDKN2A缺失状态进行分层的患者生存情况。(A)BRAF V600E突变者手术切除范围不同时的无进展生存;(B)无BRAF V600E突变者手术切除范围不同时的无进展生存;(C)不同CDKN2A情况下BRAF V600E突变者的无进展生存比较;(D)不同CDKN2A情况下无BRAF V600E突变者的无进展生存比较。GTR:手术完整切除;bal:平衡;del:缺失
为进一步验证SickKids数据中BRAF V600E突变PLGG预后差的情况,对另外18个大型儿科神经肿瘤中心的180例BRAF V600E突变PLGG病例进行了分析。总体而言,无进展生存和总生存均较差,与SickKids数据类似。此外,BRAF B600E突变PLGG中未完整切除者预后差,CDKN2A缺失者预后也较差。
结合切除范围、BRAF V600E突变、CDKN2A缺失情况,部分PLGG患者属于高危组。统计学分析表明,BRAF V600E突变和切除范围均与预后独立相关。BRAF V600E突变与CDKN2A结合考虑的话,二者联合预测复发的优势比可达3.2。与此类似,无BRAF V600E突变组切除的范围与CDKN2A的情况也是预后差的独立预测因素。SickKids数据中,具有BRAF V600E突变、且CDKN2A缺失、未完整切除者的5年无进展生存为24%,非SickKids数据中类似患者的5年无进展生存为15%。统计学分析表明,加入BRAF V600E突变可对预测模型有一定改善,生存曲线下面积从0.814增加至0.826,但无统计学意义(p=0.668)。
BRAF V600E突变、经传统治疗后出现进展的PLGG患者中有6例接受了BRAF抑制剂治疗,这6例患者对靶向治疗均有显着效果(肿瘤减小49-80%);这6例患者持续应用相关抑制剂,至今中位随访时间已达18.5个月(15-36个月)。1例患者应用2年后停药,该患者肿瘤出现了显着进展、且临床表现恶化;再次开始治疗后临床及影像学很快出现效果。对SickKids及其他数据综合分析,BRAF V600E突变患者中不论是传统化疗还是靶向治疗,6个月时肿瘤对化疗有效(肿瘤缩小>25%)的比例仅为23%;且治疗过程中高达24%的肿瘤出现了进展,由此导致治疗改变;肿瘤进展这一点在一线、二线或三线化疗中间无差别。
总之,该研究表明BRAF V600E突变的PLGG可能是一组有自身特点的肿瘤,这部分患者按照当前的辅助治疗则预后较差,相关靶向药物有望改善其治疗和预后。
点评
WHO中枢神经系统肿瘤分类最新修订版中,凸显了分子遗传学信息的重要性,这不仅体现在诊断方面,也体现在治疗及预后方面。本研究就很好的体现了分子遗传学信息对中枢神经系统肿瘤治疗和预后的重要性。
原始出处:
Lassaletta A,Zapotocky M,Mistry M,et al.Therapeutic and Prognostic Implications of BRAF V600E in Pediatric Low-Grade Gliomas[J].Journal of clinical oncology,2017.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#V600E突变#
87
#低级别胶质瘤#
78
#Oncol#
94
学习了,谢谢分享
102
#BRAF#
68
谢谢分享。
62
学习了,谢谢分享
71
学习了谢谢分享
76
学习了新知识
71
学习了谢谢分享
50