NEJM Evidence:2型糖尿病全新亚型——胰岛素清除率升高
2022-04-01 医学新视点 医学新视点
糖尿病通常分为四大类:1型、2型、特殊类型和妊娠期糖尿病,其中2型最为常见。2型糖尿病显著的病理生理学特征为
糖尿病通常分为四大类:1型、2型、特殊类型和妊娠期糖尿病,其中2型最为常见。2型糖尿病显著的病理生理学特征为胰岛素作用减弱导致的血糖代谢障碍,通常被归为两大类原因:外周胰岛素抵抗和/或胰岛素缺乏。
随着对糖尿病异质性的关注,更精准的诊疗分型也在探索中。既往已有研究提出,在2型糖尿病中,胰岛素缺乏的病因除了普遍认为的胰腺β细胞退化导致胰岛素分泌减少,也包括胰岛素清除率升高和胰岛素降解能力增加等。
近日,发表于《新英格兰医学杂志-循证》(NEJM Evidence)的一项研究对此进一步探索,识别出一组以胰岛素清除率升高为病理生理学特征的2型糖尿病患者,分析这部分患者的临床特征发现,他们通常不胖,β细胞胰岛素分泌功能良好,胰岛素敏感性甚至更好,但胰岛素水平更低、空腹血糖更高。
论文指出,如果这种全新的亚型得到进一步验证,可能将为这部分患者的精准治疗带来改变。
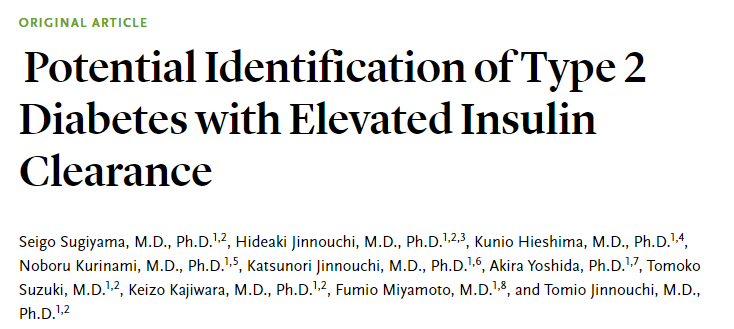
截图来源:NEJM Evidence
这项成果来自日本的糖尿病医疗团队。此前,研究团队已经报道了1例空腹血胰岛素浓度降低、胰岛素清除率升高的2型糖尿病。此次研究团队对更多患者展开了分析,在日本熊本市的阵内医院(Jinnouchi Hospital)糖尿病诊疗中心招募了101名新诊断、未接受过治疗的2型糖尿病患者(78.2%为男性,平均54.1岁)。选择这些患者,是考虑他们通常没有晚期、严重的胰腺β细胞功能障碍。
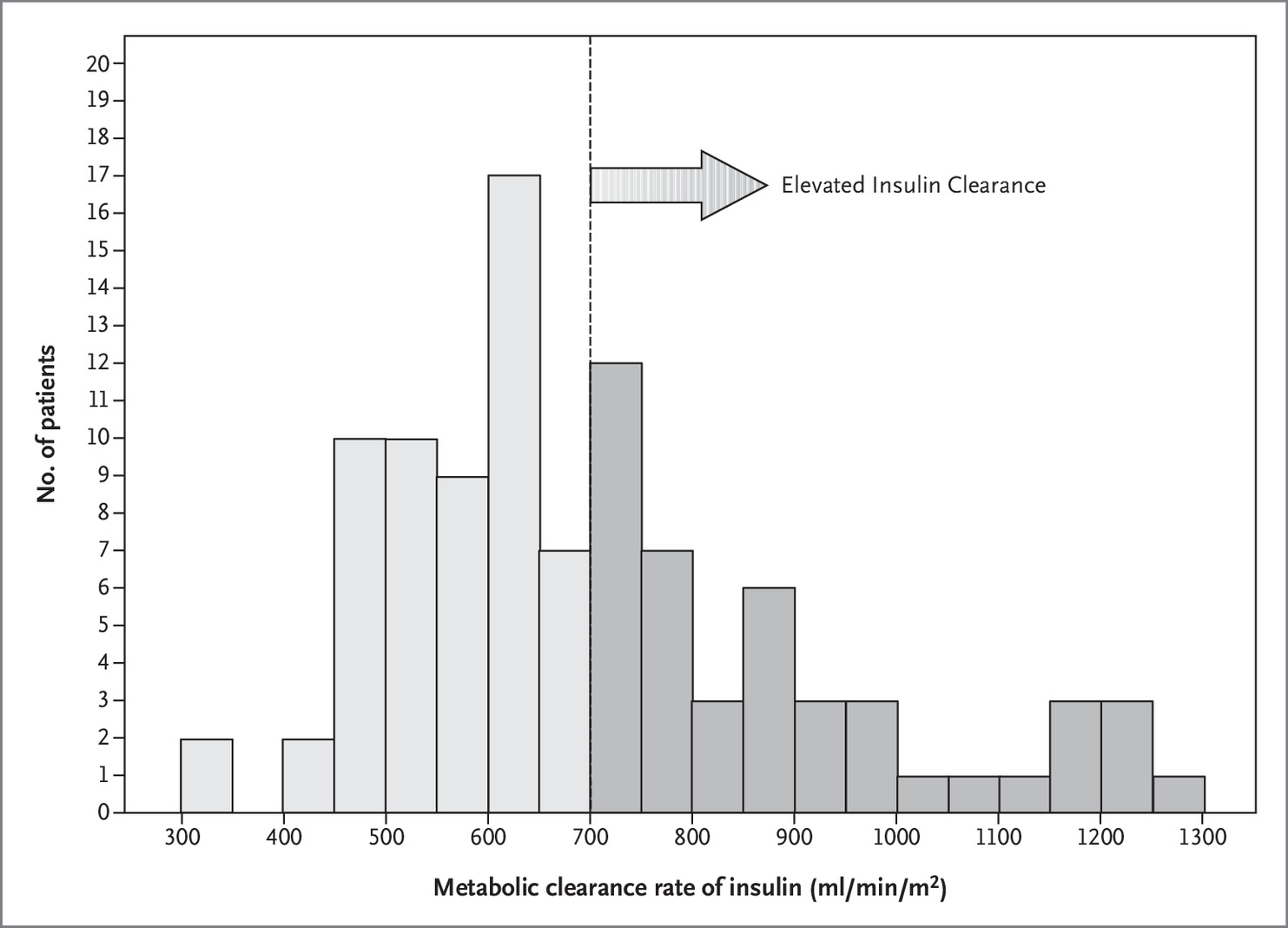
研究者通过高胰岛素-正常血糖钳夹实验来评估了患者的胰岛素代谢清除率(MCRI),并参考既往研究数据将胰岛素清除率升高定义为MCRI>700 ml/min/m2。
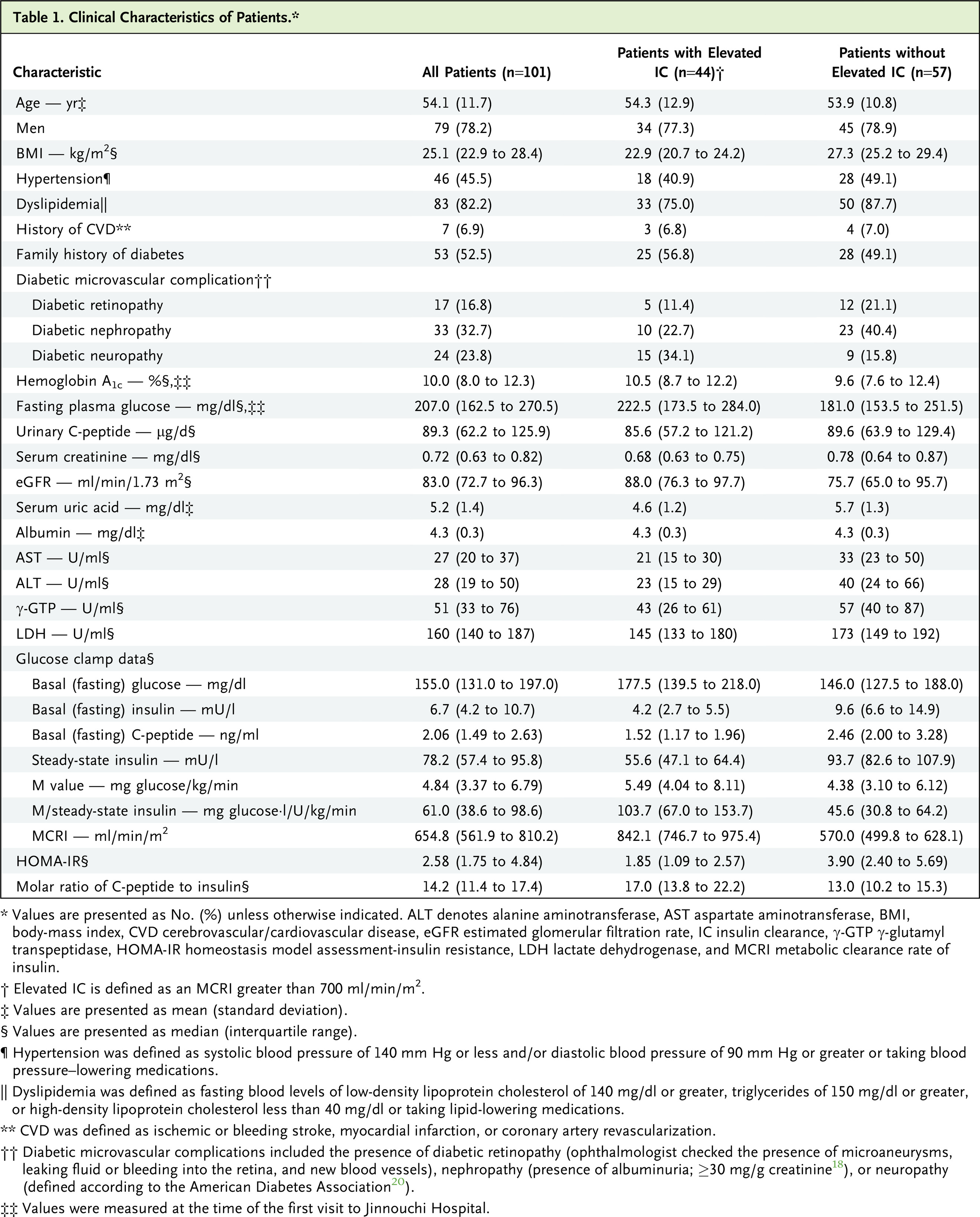
共有44例(44%)患者属于胰岛素清除率升高,MCRI中位值明显高于其他患者(842 ml/min/m2 vs 570 ml/min/m2)。相比胰岛素清除率未增加的患者,胰岛素清除率升高的患者有一些明显的临床特征:
-
尽管年龄、性别没有显著差异,但他们通常并不肥胖,体重指数[BMI]中位值22.9 kg/m2 vs 27.3 kg/m2;
-
这些人群的空腹血糖更高(中位值178 mg/dl vs 146 mg/dl),空腹血清胰岛素水平更低(4.2 mU/l vs 9.6 mU/l),但糖化血红蛋白(HbA1c)水平相似。
-
他们仍然具有良好的胰岛素敏感性,稳态葡萄糖输注速率/稳态胰岛素的中位值显著更高(103.7 mg 葡萄糖⋅l/U/kg/min vs 45.6 mg 葡萄糖⋅l/U/kg/min),HOMA-IR值更低(1.85 vs 3.9);胰腺β细胞胰岛素分泌功能也保留较好(每日尿C肽排泄量相似,中位值85.6 μg/天 vs 89.6μg/天)。
-
两组患者的糖尿病病程、糖尿病家族史百分比、糖尿病视网膜病变、肾或肝功能检查结果没有显著的临床差异。
基于血糖和胰岛素相关指标,研究团队推测,这些患者的高血糖是由胰岛素清除率升高所引起的,而不是由胰岛素抵抗所引起的。这与欧美患者的常见情况恰恰相反。欧美地区的2型糖尿病患者更多表现为高胰岛素血症(由于胰岛素清除率降低,以及肥胖相关的胰岛素敏感性降低)。
论文进一步讨论指出,胰岛素清除率可能受到基因调控,已有研究报道日本人群的肝脏胰岛素清除率高于白种人和墨西哥裔。肝脏中的胰岛素清除过程,会将胰腺β细胞分泌的一半以上的胰岛素降解到肝脏门静脉中。此外,尽管有研究提示肝细胞损伤可能会减弱肝脏对胰岛素的清除,但这项研究中近1/3肝转氨酶升高的患者存在胰岛素清除增加的现象,这提示,肝外器官中也可能发生胰岛素清除增加。
研究团队也提出了本研究中的一些局限性,包括样本量小,以及是单中心研究,难免有选择偏倚。此外,只招募了新诊断为 T2DM 的初治患者。因为我们没有测量或评估胰腺 β 细胞的胰岛素分泌(例如,通过高血糖钳)或生理刺激(例如,通过口服葡萄糖耐量试验),所以我们不知道胰腺 β 细胞的胰岛素分泌反应是否目前研究中升高的IC是正常的。需要进一步研究 IC 升高的 T2DM 患者的胰岛素分泌反应的细节,包括对肝葡萄糖产生和肝胰岛素敏感性的研究。但总体而言,这项研究提示,在这种新识别的2型糖尿病亚型中,胰岛素清除率升高(IC)导致的胰岛素作用障碍是重要发病机制,但是并没有确定因果关系,未来期待更多研究对此进行验证。
同期还配了编辑评论:Precision Diagnostics for Type 2 Diabetes Mellitus — Have We Arrived?认为2 型糖尿病 (T2DM) 由一个共同的终点定义:空腹血糖诊断为高血糖,口服葡萄糖耐量试验期间的血糖,或没有自身免疫性 β 细胞破坏的血红蛋白 A1c升高。 从历史上看,很少关注导致高血糖的病因; 因此,缺乏一种优雅的病理生理学指导的诊断和治疗方法。 T2DM 被简单地认为是胰岛素缺乏和/或外周胰岛素抵抗的结果。 然而,T2DM 的表型是异质的,病理生理学也是异质的。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#胰岛#
99
很好
78
学习了
85
学习了
102
认真学习~~
93