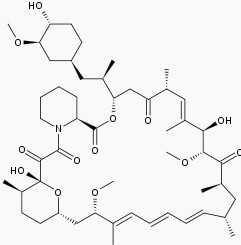
CHEST:西罗莫司和自噬抑制对LAM治疗效果的I期临床试验
2017-02-15 MedSci MedSci原创
动物和细胞研究支持抑制自噬在淋巴管平滑肌瘤病(LAM)中的重要性。近期,一项发表在杂志CHEST上的研究在具有LAM的受试者队列中,测试了2种不同剂量水平下使用西罗莫司和羟基氯喹(自噬抑制剂)治疗的安全性和耐受性。此外还研究了肺功能的变化。此项为期48周、2个中心的I期试验评估了予以≥18岁的LAM患者每日两次逐渐增高的口服羟氯喹剂量(100-200mg)联合西罗莫司的安全性。受试者接受联合治疗2
动物和细胞研究支持抑制自噬在淋巴管平滑肌瘤病(LAM)中的重要性。
近期,一项发表在杂志CHEST上的研究在具有LAM的受试者队列中,测试了2种不同剂量水平下使用西罗莫司和羟基氯喹(自噬抑制剂)治疗的安全性和耐受性。此外还研究了肺功能的变化。
此项为期48周、2个中心的I期试验评估了予以≥18岁的LAM患者每日两次逐渐增高的口服羟氯喹剂量(100-200mg)联合西罗莫司的安全性。受试者接受联合治疗24周,然后停止药物进行为期24周的观察研究。
此项研究结果表明,共14名患者提供书面知情同意书。最常见的不良事件是粘膜炎、头痛和腹泻。没有与药物相关的严重不良事件的报告。次要终点显示24周时肺功能得到改善,48周时肺功能降低。当分别分析较高剂量的羟氯喹时,FEV1和FVC在48周保持稳定,但是6分钟步行距离减少。
此项研究结果表明:每天两次200mg的西罗莫司和羟氯喹的组合具有良好的耐受性,没有发生剂量限制性不良事件。尚需在更大的试验中探讨对肺功能的潜在影响。
原始出处:
El-Chemaly S, Taveira-Dasilva A, Goldberg HJ, et al. Sirolimus and Autophagy Inhibition in LAM: Results of a Phase I Clinical Trial. Chest. 2017 Feb 10. pii: S0012-3692(17)30174-5. doi: 10.1016/j.chest.2017.01.033.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#I期临床#
48
#I期临床试验#
54
#EST#
51
#治疗效果#
55
#Chest#
61
#LAM#
54
#西罗莫司#
0
文章真心不错耶
109