80%的直肠癌会被误认为痔疮!同为便血该如何鉴别?
2022-02-02 胃肠病 胃肠病
临床上经常会遇到病人一有少量便血即想到自己是否得了不治之症,整天忧心忡忡,直到医院彻底检查后才如释重担,那么两者有没有鉴别点,本文将给大家作以简要介绍。
临床上经常会遇到病人一有少量便血即想到自己是否得了不治之症,整天忧心忡忡,直到医院彻底检查后才如释重担,那么两者有没有鉴别点,本文将给大家作以简要介绍。
80%的直肠癌曾被误诊为痔疮
小王是一个帅气的小伙子,今年刚满30岁,是一个政府公务员,有一个幸福的家庭,妻子贤惠美丽,3岁的儿子活泼可爱。一年前,开始大便带鲜血,认为是痔疮,陆陆续续食用了不少治疗痔疮的药物,时好时歹,淅淅沥沥,总不断根。
在肛肠科大夫的一再劝说下,才不情愿地来我们内镜中心做肠镜检查。
检查前,小王还满不在乎,信誓旦旦地说:“我这就是痔疮,肯定没别的事儿,有必要做肠镜么?”
结果,镜子刚进了10 cm,就看到以下这个样子了:
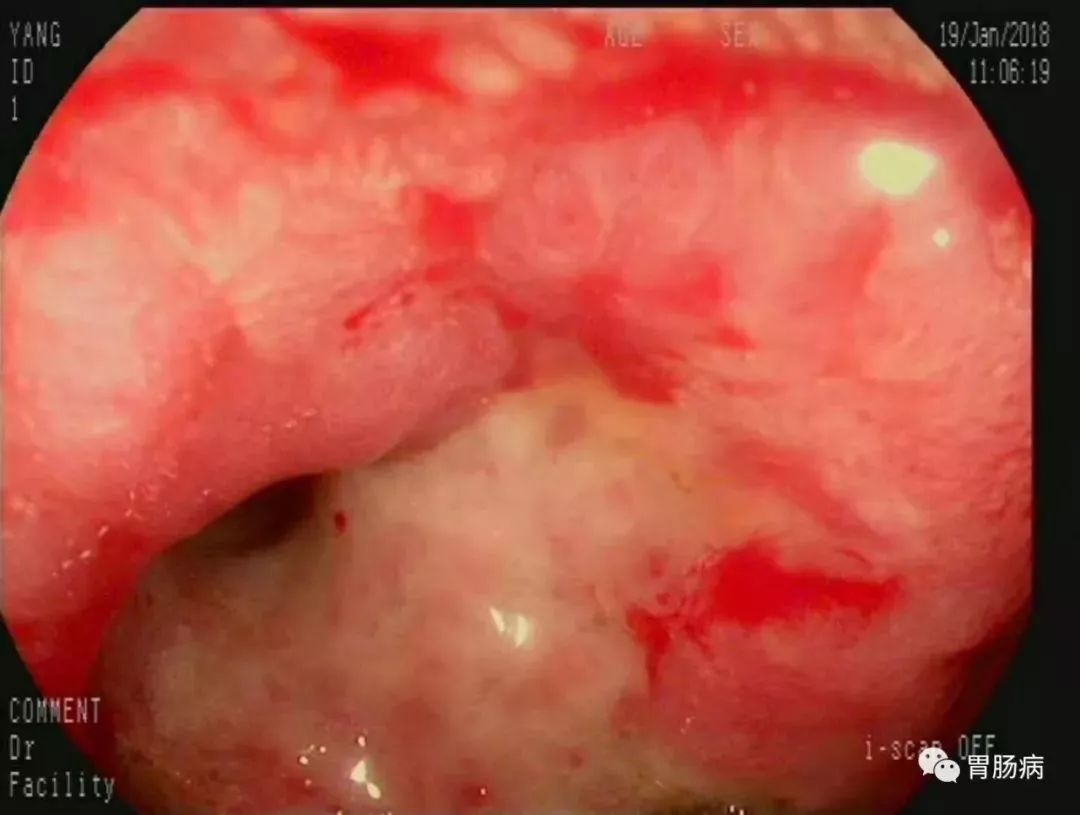
当时考虑低分化浸润癌,病理结果出来了:“(直肠距肛缘10 cm处)小细胞恶性肿瘤,倾向于低分化癌,建议免疫组化进一步分类”。
且不说,小王的妻子如何面对这一结果,三岁的儿子情何以堪,令人扼腕叹息的是,如果在便血初期,不自以为是,及时咨询医生,做个肠镜,就会免此大祸。
痔疮和直肠癌都会引起便血
痔疮是直肠下段、肛管和肛门缘的静脉丛曲张所形成的静脉团,属于人体“突起”病变,痔疮的本质是血管团。
因此,其出血主要是各种原因(如久坐、免疫力下降、长期口服抗凝药、饮酒、辛辣刺激等)导致血管团局部破损所致。
直肠癌属于恶性肿瘤,是人体的“异常组织”。直肠癌的本质是肿瘤细胞和供应肿瘤细胞的小血管。
因此,其出血来源多是癌浸润直肠黏膜使其表面溃烂或癌肿本身破溃导致。
一、便血特点鉴别
1、痔疮的便血特点:
痔疮便血的特点是排便中或便后出血,色鲜红,如图:

痔疮分内痔、外痔、混合痔、肛裂等;
外痔一般不出血,内痔出血但一般不疼痛,大多是点滴状、线状、或喷射状,颜色大多呈鲜红色有时大便表面附有少量血液或将手纸染红,有时为滴血,便后出血多自行停止。
若长期反复出血或多次大量出血,还可引起贫血。
2、直肠癌的出血特点
直肠癌出血的特点是血与大便相混合,便血呈暗红色,又称为果酱样便,如图:

出血根据病变部位距肛门的距离远近,可能是鲜红色,也可能是暗红色,靠上部位的结肠癌也可能出现铁锈色甚至黑色。
它的特点是有伴随症状:
比如,排便习惯的改变,次数增加,排便不尽感、腹泻、便秘交替,伴有黏液或脓血等等。
需要注意的是,有时仅为大便表面黏血迹,也有的会是鲜血。 这一点很难与痔疮相区别。
3.息肉出血
某些息肉也会出血。也是看息肉距肛门的远近,近的呈鲜红色,远的是暗红色;一般没有伴随症状。
4.肛裂出血
肛裂伴有周期性疼痛,便前疼痛剧烈,便后稍缓解,后又继续疼痛,它的出血也是鲜红色的,类似于内痔出血。
二、伴随症状不同
某些息肉也会出血。也是看息肉距肛门的远近,近的呈鲜红色,远的是暗红色;一般没有伴随症状。
1、痔疮除便血外还有以下症状:
①内痔脱出:
早期仅有便血,没有脱出;
二期内痔伴有排便脱出,便后能自行回纳;
三期不能自行回纳,须用手回纳,甚至在用力或咳嗽时均可脱出。
②疼痛:内痔一般无疼痛,如果内痔嵌顿(即脱出后“卡”在肛门不能回纳)可出现剧烈疼痛。
③肛门瘙痒。三期以上内痔因括约肌松弛,肠腔内分泌物流出,可致肛门周围潮湿瘙痒。
④肛门坠胀。肿大的痔核刺激直肠黏膜或痔黏膜表面炎症引起肛门坠胀。
2、直肠癌伴随症状较多,主要症状有:
①直肠刺激症状。常见腹泻,里急后重及排便不尽感,有时每日排便数次,但每次量不多。部分患者可表现为腹泻及便秘交替出现。
②癌肿破溃感染症状。常见大便带有脓血及黏液,一般出血量较少,血呈鲜红色或稍暗,附于大便表面,便血常为间歇性,少数病例可发生大量出血,病人有肛门下坠不适感。
③肠腔狭窄梗阻症状。癌肿浸润肠壁使肠腔狭窄,引起大便变细变形,严重时出现排便困难。
④消耗征象。恶性肿瘤长期慢性消耗,可出现贫血、消瘦等恶病质征象。
⑤转移征象。直肠癌一般无疼痛,但癌肿浸润肛管和括约肌则疼痛显著,恶性肿瘤细胞可以随血液淋巴转移至其他部位,如肝脏,肺等。
也可直接浸润到临近的组织,如尿道,阴道,前列腺等,产生相应部位的症状。
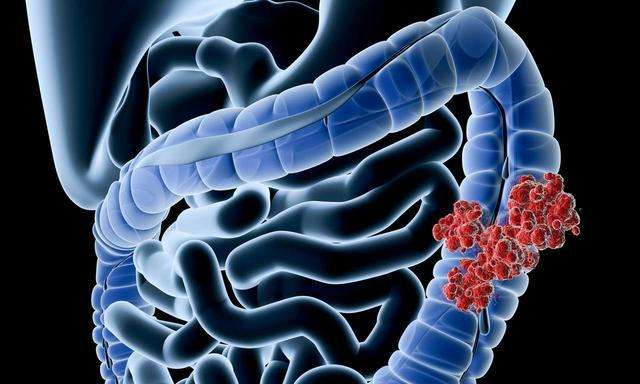
附直肠癌图片:

三、好发年龄
痔疮任何年龄均可发作,但随年龄增长发病率增高。
直肠癌好发于中年人或老年人。但近年来也有年轻化趋势,30岁以下人群屡见不鲜。
所以任何年龄段的便血,都不能轻心大意!
四、主要靠检查来鉴别
鉴别痔疮与直肠癌,主要靠医生检查。
1、肛门指检
一般肛门指诊非常重要,因为大部分的痔疮和直肠癌都是发生于手指可以触及的部位。
如果用手指由肛门伸入触之,感到内部有柔软突起,表面光滑无压痛的黏膜结节则为痔疮。
如果感到肠内有形状不规则边缘不整齐表面不光滑的菜花硬块或边缘隆起中央凹陷的溃疡,并发现肠腔狭窄得仅能容纳一个手指;
检查后,指套上沾有血液、黏液者,则极可能患上了直肠癌。
2、肠镜检查
其次需要医生用专门的检查设备,如喇叭口肛门镜,电子直肠镜、电子纤维结肠镜等,这些检查要求病人排净大便甚或清洁肠道以便直视下辨别是否为痔疮还是肿瘤。
特别提示
如果您大便带血,千万不能掉以轻心,一定要到找专科医生进行检查,以排除直肠癌的可能。
因为,80%以上的直肠癌首次就诊会被误诊为痔疮!
即使是医生明确了痔疮出血,如果用药一段时间后仍然有便血时更要注意进一步检查,以免“癌瘤出血”被“痔疮出血”所掩盖而耽误了治疗时机。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










基本科普很详细
94
这个#科普#非常有必要!
123
#直肠癌#
146
#痔疮#
92
#便血#
116
对
1