Lenzilumab治疗COVID-19住院患者,即将开展III期临床
2021-01-31 Allan MedSci原创
生物制药公司Humanigen近日宣布,已完成Lenzilumab治疗COVID-19住院患者的III期研究入组工作。该公司预计将于2021年3月公布主要临床数据。
生物制药公司Humanigen近日宣布,已完成Lenzilumab治疗COVID-19住院患者的III期研究入组工作。该公司预计将于2021年3月公布主要临床数据。

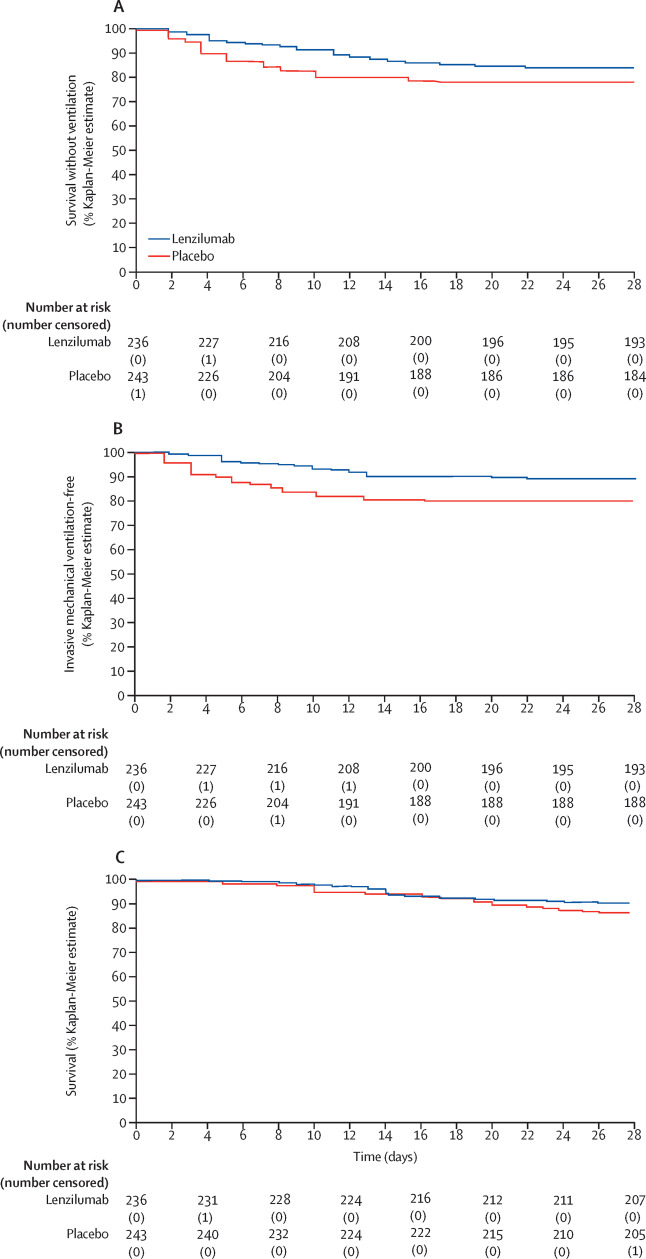
这项III期随机、双盲、安慰剂对照临床试验招募了520例患者,其主要目标是确定lenzilumab能否缓解免疫介导的细胞因子释放综合征(CRS)并改善COVID-19住院和低氧患者的无呼吸机生存。
Humanigen首席执行官Cameron Durrant博士说:“完成这项III期研究的入组是lenzilumab临床开发的重要里程碑。与疫苗一起使用的药物是治疗COVID-19的重要工具。我们感谢试验参与者、研究人员和医疗保健专业人员在促进lenzilumab的方面所做出的贡献”。
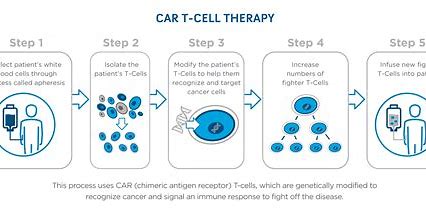
Lenzilumab是一种抗人类粒细胞巨噬细胞集落刺激因子(GM-CSF)单克隆抗体,旨在预防和治疗细胞因子风暴,这种并发症被认为是引起急性呼吸窘迫综合征(ARDS)的原因,并可能导致某些COVID-19患者死亡。数据显示,近90%的COVID-19住院患者有罹患细胞因子风暴的风险。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#I期临床#
71
#III#
64
#mAb#
54
#II期临床#
59
#III期#
76