Blood:在贫血恢复过程中,单核细胞来源的巨噬细胞可扩张小鼠应激性红细胞壁龛
2018-10-22 MedSci MedSci原创
中心点:在贫血的恢复过程中,单核细胞被招募到脾脏生成巨噬细胞,进而形成应激性红细胞壁龛。单核细胞成熟形成巨噬细胞与应激性红系祖细胞发育平行发生。摘要:贫血应激会诱导一系列生理反应,包括快速产生新的红细胞,该过程被称为应激性红系发生。在小鼠中该过程很好理解,因为它发生在骨髓外,采用的信号和祖细胞不同与骨髓稳定状态的红系发生。应激性红系祖细胞的发育与脾脏应激性红细胞壁龛密切相关。特别是适度的应激性红系
在贫血的恢复过程中,单核细胞被招募到脾脏生成巨噬细胞,进而形成应激性红细胞壁龛。
单核细胞成熟形成巨噬细胞与应激性红系祖细胞发育平行发生。
摘要:
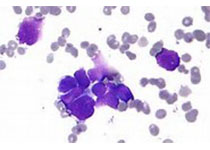
贫血应激会诱导一系列生理反应,包括快速产生新的红细胞,该过程被称为应激性红系发生。在小鼠中该过程很好理解,因为它发生在骨髓外,采用的信号和祖细胞不同与骨髓稳定状态的红系发生。应激性红系祖细胞的发育与脾脏应激性红细胞壁龛密切相关。特别是适度的应激性红系发生需要壁龛中的巨噬细胞参与。
研究人员发现随着应激性红系祖细胞的增殖和分化,壁龛的扩张也随之发生。在两种贫血应激模型中采用谱系示踪分析发现,脾脏壁龛扩张是由于单核细胞被招募到脾脏,随后变成巨噬细胞形成红细胞岛。单核细胞流入脾脏部分依赖于由Ccl2和脾脏常驻红髓巨噬细胞所表达的其他配体介导的Ccr2依赖性信号。
总而言之,本研究阐明了脾脏壁龛的动态特性,即在贫血应激的情况下,与应激性红系祖细胞一起迅速扩张,协调产生新的红细胞。
Chang Liao, K. Sandeep Prabhu, and Robert F. Paulson.Monocyte derived macrophages expand the murine stress erythropoietic niche during the recovery from anemia.Blood 2018 :blood-2018-06-856831; doi: https://doi.org/10.1182/blood-2018-06-856831
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#扩张#
56
#红细胞#
65
#单核细胞#
74
#应激#
75