Dig Liver Dis: 荟萃分析:抗TNFα药物是预防术后克罗恩病的更佳选择
2019-07-07 不详 MedSci原创
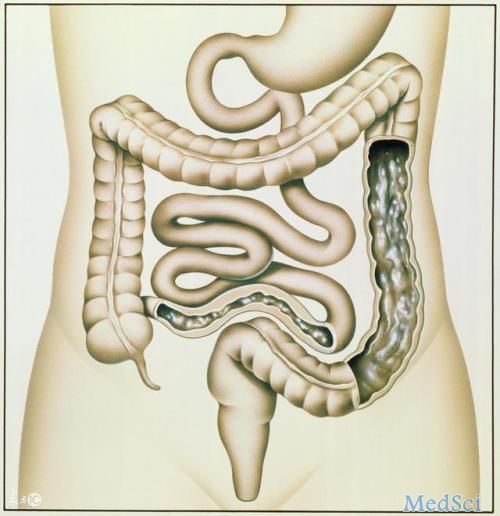
尽管克罗恩病(CD)的术后复发率(POR)很高,但其预防达策略还未达成共识。本项研究的目的是比较生物疗法和常规疗法在预防CD的POR方面的功效。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#TNFα#
79
#荟萃分析#
50
#抗TNF#
58
#荟萃#
67
#Dis#
72
#TNF#
68
学习了,谢谢分享。
116