在一项新的研究中,来自汉诺威医学院的研究人员让一名患有重症肺动脉高压(pulmonary hypertension, PAH)的三岁女孩接受了从人类脐带血中获得的间充质干细胞(MSC)产物共五次治疗,首次成功地阻止了通常致命的肺动脉高压过程。
相关研究结果于2022年6月9日在线发表在Nature Cardiovascular Research期刊上,论文标题为“Human umbilical cord mesenchymal stem cell-derived treatment of severe pulmonary arterial hypertension”。
论文通讯作者、汉诺威医学院转化心肺生物医学研究组组长Georg Hansmann教授说,“这种治疗导致生长、运动耐力和临床心血管变量的明显改善,并减少了血液中可检测到的血管收缩和炎症的血浆标志物数量。6个月后,不仅健康状况有了明显的改善,而且也没有出现不良的副作用。”
这是第一次有针对患有明显的肺动脉高压的人的疗法。Hansmann教授强调说,“还需要进一步研究,以确认和探索这种新的干细胞疗法的好处。”
肺动脉高压是一种疾病,肺循环中的血压长期升高,因此被称为肺动脉高压。导致肺动脉高压的原因通常是肺部血管狭窄和/或这些血管的损失。这种疾病是渐进的,通常是致命的。在晚期阶段,肺动脉高压被认为是无法治愈的。目前批准的抗肺动脉高压药物主要是针对血管扩张。
重复间质干细胞疗法是基于新生儿脐带血的间质干细胞,即人脐带血间质干细胞(human umbilical cord mesenchymal stem cell, HUCMSC)。这些作者的分析表明,这些脐带血干细胞的产物能够改善受损血管的再生,抑制血管的炎症,并遏制某些部位的细胞损伤。
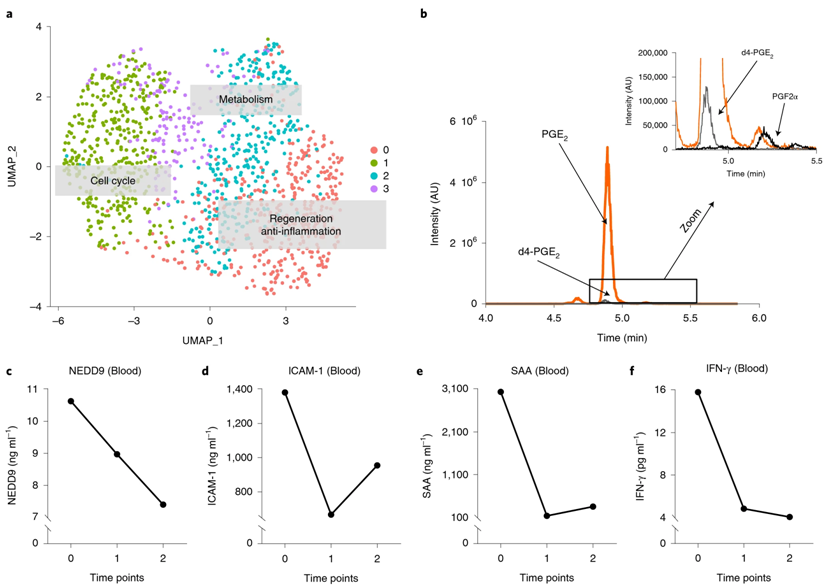
对HUCMSC的scRNA-seq分析揭示四个MSC细胞团以及再生、抗炎症、细胞周期和代谢增强的转录组。图片来自Nature Cardiovascular Research, 2022, doi:10.1038/s44161-022-00083-z。
Hansmann教授解释说,“我们有证据表明这种HUCMSC衍生性疗法有多种有益效果:在接受治疗的患者心脏中,它主要保护提供能量的线粒体,而在肺部,这种治疗主要是抑制炎症和刺激再生。我们可以发现蛋白、脂质和前列腺素E2在HUCMSC及其产物中富集,而且这种HUCMSC衍生性疗法能同时调节PAH的几个关键信号通路。”
这种如今发表的新治疗方法是通过Hansmann教授和汉诺威医学院妇产科的Ralf Hass教授博士之间的合作实现的。一个由科学家、研究员和医生组成的非常大的团队帮助实施了这个 “个体治愈实验”。Hansmann教授将由此产生的间充质干细胞的条件培养液两次在心脏导管插入术实验室中直接注入肺动脉,三次通过中心静脉注入肺动脉。
Hansmann教授的研究团队与莱顿大学和柏林夏里特医院的合作伙伴,对来自多种脐带血的间充质干细胞及其产物进行了进一步的所谓组学分析。Hansmann教授通过2011年和2012年在美国波士顿哈佛大学医学院进行的动物间充质干细胞的初步实验,以及他的汉诺威医学院研究组进行的体内实验和这名女孩的父母的请求,最终提出了这种治疗肺动脉高压的新方法。
Has教授的妇产科研究团队多年来一直在研究间质干细胞,并发表了关于它们在受损和病理生理组织中的特定再生特性和效果的文章。利用一种特殊的技术,Hass教授能够从脐带组织中分离出间充质干细胞,并在细胞培养液中充分增殖,从而使它们随后能够用于治疗。
这些作者认为,对于慢性进展的、往往是治疗抵抗性的肺动脉高压,这样的治疗必须定期重复,才能取得长期的成功。
参考资料:
Georg Hansmann et al. Human umbilical cord mesenchymal stem cell-derived treatment of severe pulmonary arterial hypertension. Nature Cardiovascular Research, 2022, doi:10.1038/s44161-022-00083-z.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Nat#
77
#动脉高压#
90
#肺动脉高压患者#
109
#间充质干细#
82
#脐带血#
129
#脐带#
74
希望干细胞更好的服务于人民
80