Kidney Int :达格列净和预防慢性肾脏疾病不良结局(DAPA-CKD)预先指定分析对肾功能突然下降发生率的随机对照试验研究
2021-11-04 从医路漫漫 MedSci原创
钠-葡萄糖共转运体2 (SGLT2)抑制剂可以延缓肾功能下降的进展,并降低肾衰竭的风险。
全球每年约有1300万人发生急性肾损伤(AKI),主要发生在住院患者中。尽管众所周知,严重的慢性肾脏疾病(CKD)与AKI风险升高相关,但来自大型流行病学研究的新数据表明,AKI发作也会增加CKD进展的风险。此外,AKI与不良临床结局相关,包括透析、心血管疾病和死亡率,尤其是糖尿病患者和有显性蛋白尿的患者。在2型糖尿病患者中进行的大型随机对照试验显示,钠-葡萄糖共转运体2 (SGLT2)抑制剂可以延缓肾功能下降的进展,并降低肾衰竭的风险。在SGLT2抑制剂应用的早期阶段,人们担心这些药物会增加因低血容量、治疗引起的急性肾小球滤过率(GFR)降低而导致的AKI风险,并有可能引发肾髓质缺氧损伤。这些担忧得到了早期病例报告的支持,这些报告表明,在2型糖尿病患者中,使用SGLT2抑制剂并保持肾功能的患者发生AKI的风险更高。然而,大型心血管和肾脏结局试验表明,SGLT2抑制剂实际上可以降低AKI的风险。多个试验的一致性表明,这是一种分级效应,并不局限于特定的SGLT2抑制剂。此外,后续的研究已经确定了SGLT2抑制可以降低AKI风险的机制。
了解CKD和蛋白尿患者中SGLT2抑制与AKI风险之间的关系是很重要的,因为CKD患者的AKI发生率高于肾功能正常或接近正常的患者。达格列净和预防慢性肾脏疾病不良结局(DAPA-CKD)试验表明,SGLT2抑制剂达格列净降低了合并和不合并2型糖尿病的CKD患者肾衰竭和心力衰竭住院的风险,延长了患者的生存期。在这项研究中,我们报道了达格列净对肾功能突然下降的影响,并记录在DAPA-CKD试验中,作为预先指定的探索性结果,定义为后续两次就诊之间血清肌酐增加一倍。我们还比较了随机接受达格列净或安慰剂治疗的患者严重AKI不良事件的发生率(根据研究人员的报告)。
方法:DAPA-CKD是一项随机、双盲、安慰剂对照试验,平均随访时间为2.4年。将患有慢性肾脏病(尿白蛋白/肌酐比值200-5000 mg/g,估计肾小球滤过率为25-75mL/min/1.73m2)的成年人随机分成两组,分别服用达格列净10 mg/d和安慰剂(每组2152人)。这种治疗将一直持续到糖尿病酮症酸中毒、怀孕、不接受治疗或研究完成。随机分组后,在2周、2、4和8个月进行随访,此后每隔4个月进行一次随访。在每次随访中,记录生命体征,送血样和尿样进行实验室评估,并收集关于潜在研究终点、不良事件、其他治疗和研究药物依从性的信息。肾功能的突然下降被定义为在随后的两次随访期间血清肌酐增加一倍到达预先指定的终点。我们还评估了研究人员报告的急性肾损伤相关严重不良事件的事后分析。
结果:达格列净组和安慰剂组分别有63人(2.9%)和91人(4.2%)在随后两次就诊期间(中位时间间隔100天)血肌酐增加一倍(危险比0.68[95%可信区间0.49,0.94])。对死亡风险的考虑并没有改变我们的研究结果。基于基线亚组,达格列净对肾功能突然下降的影响无显著差异。急性肾损伤相关的严重不良事件在达格列净组和安慰剂组分别为52例(2.5%)和69例(3.2%),差异无统计学意义(0.77[0.54,1.10])。

图1 所示为肾功能突然下降的累积发病率曲线(以100天为间隔的中位数就诊之间血清肌酐至少增加一倍)。提供的是Aalen-Johansen累积发病率估计值,其中考虑了相互竞争的死亡率风险。CI,置信区间。

图2 森林图显示了按亚组划分的肾功能突然下降的发生率(以平均100天为间隔的访视期间血清肌酐至少翻倍)。CI,置信区间;eGFR,估计肾小球滤过率;UACR:尿白蛋白与肌酐的比值。

表1 影响肾功能突然下降事件相关的因素

表2 肾功能突然下降与ESKD/肾死亡和死亡率之间的关系
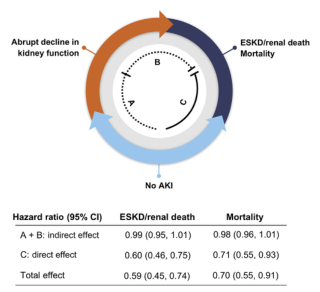
图3 通过达格列净治疗对终末期肾病(ESKD)或肾功能突然下降的全因死亡结局的调节作用。
结论:在CKD和大量蛋白尿的患者中,达格列净降低了肾功能突然下降的风险。
原文出处:
Heerspink HJ, Cherney D, Postmus D,et al.A pre-specified analysis of the Dapagliflozin and Prevention of Adverse Outcomes in Chronic Kidney Disease (DAPA-CKD) randomized controlled trial on the incidence of abrupt declines in kidney function.Kidney Int 2021 Sep 21
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#对照试验#
158
#肾功能#
100
#发生率#
65
#对照#
70
#随机对照试验#
83
#APA#
78
#kidney#
88
#慢性肾脏#
98
学习
86
#学习#
113