Breast Cancer Res.:低ATM蛋白表达与激素阴性乳腺癌预后不良有关
2015-05-08 范伟译 MedSci原创
背景:丝氨酸/苏氨酸蛋白激酶共济失调症突变蛋白(ATM)在维持基因组的完整性上是至关重要的。双链DNA的断裂,ATM磷酸化关键的下调蛋白质包括p53和BRCA1/2,编码着复杂的信号通路参与细胞周期停滞、DNA修复、衰老和凋亡。虽然ATM零星的突变很少发生在乳腺癌,在乳腺癌中其蛋白表达的状态及其临床意义仍不完善。我们的研究旨在调研在激素阳性(HPBC)和激素阴性(HNBC)早期乳腺癌(EBC)中,
背景:丝氨酸/苏氨酸蛋白激酶共济失调症突变蛋白(ATM)在维持基因组的完整性上是至关重要的。双链DNA的断裂,ATM磷酸化关键的下调蛋白质包括p53和BRCA1/2,编码着复杂的信号通路参与细胞周期停滞、DNA修复、衰老和凋亡。虽然ATM零星的突变很少发生在乳腺癌,在乳腺癌中其蛋白表达的状态及其临床意义仍不完善。我们的研究旨在调研在激素阳性(HPBC)和激素阴性(HNBC)早期乳腺癌(EBC)中,ATM蛋白对肿瘤和癌症相关的基质在临床结果上的影响。
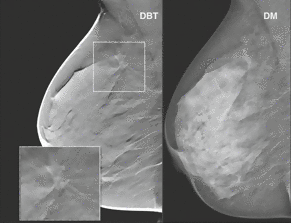
方法:组织微阵列(TMA),包含加拿大卡尔加里汤姆贝克癌症中心诊断的肿瘤患者,福尔马林保存、石蜡嵌入式切除的两组患者的肿瘤(HPBC组:n = 130;HNBC组:n = 168),采用荧光免疫组织化学(IHC)和自动定量分析(AQUA)对ATM的蛋白表达进行分析。ATM的表达水平测定在整个肿瘤(tATM)由pan-细胞角蛋白表达标示,肿瘤核舱(nATM)由DAPI和pan-细胞角蛋白阳性标示,癌症相关基质(csATM)由波形蛋白-阳性和pan-细胞角蛋白-阴性标示。ATM在这些不同部分内的表达水平与临床结果相关。
结果:然而相比正常乳腺上皮组织,tATM和nATM在肿瘤组织显著降低,csATM明显高于相应的正常组织。此外,在tATM和nATM的平均表达水平在HNBC 和HPBC中降低了两到三倍(p < 0.001)。在HNBC和HPBC组,患者较低表达的tATM,nATM和csATM肿瘤相比那些较高的tATM,nATM和csATM肿瘤有着明显较差的生存结果,这在HNBC组效果更加明显。多变量分析表明,只有在HNBC组(p < 0.001),这些生物标记物预测存活的独立指标有肿瘤大小、淋巴结状态。
结论:在恶性肿瘤和基质隔间较低的ATM蛋白表达可能导致乳腺癌有天然的侵略性,对于较差生存期的HNBC患者它也是独立的预后因素。
原始出处:
Feng X1, Li H2,3, Dean M4,5, Wilson HE6,7, Kornaga E8,9, Enwere E10,11, Tang P12, Paterson A13, Lees-Miller SP14, Magliocco AM15,16,17,18, Bebb G19.Low ATM protein expression in malignant tumor as well as cancer-associated stroma are independent prognostic factors in a retrospective study of early stage hormone negative breast cancer.Breast Cancer Res. 2015 May 3;17(1):65.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#AST#
61
#阴性乳腺癌#
69
#Res.:#
54
#M蛋白#
92
期待有更多研究
16
#ATM蛋白#
53
#Breast#
60
#预后不良#
47
#蛋白表达#
64
看看
137