NEJM:创伤性枢椎滑脱-案例报道
2017-05-04 xing.T MedSci原创
创伤性枢椎滑脱,亦称Hangman骨折,是由颈部过度牵张引起的。这些骨折是根据前后位移偏差程度、有无后纵韧带断裂、骨折线的位置以及有无小关节脱位的存在来进行分类。
患者为一名25岁的男性,因交通事故后出现严重颈部疼痛而到急诊就诊。该患者的手臂和大腿有力,轻触觉和针刺觉正常,无括约肌障碍。
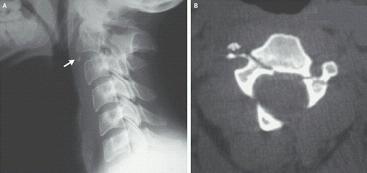
侧位片(如图A)显示,C2和C3椎体之间的椎间盘破裂,C2椎体后角成为碎片,左侧椎弓根轴向骨折,并伴有前下部位有一个小碎片(如图中箭头所示)。轴向断层扫描(如图B)确认为右侧和左侧C2椎体左椎弓根骨折。
创伤性枢椎滑脱,亦称Hangman骨折,是由颈部过度牵张引起的。这些骨折是根据前后位移偏差程度、有无后纵韧带断裂、骨折线的位置以及有无小关节脱位的存在来进行分类。
稳定骨折同时位移最小的情况可能通过外部固定进行保守治疗,但对于不稳定的骨折,正如这个患者,需要手术进行固定。
该患者接受了C2和C3椎骨的前路融合术,并在随访4年后,该患者没有神经功能缺损以及疼痛。
原始出处:
Anis Khelifi,et al. Traumatic Spondylolisthesis of the Axis.N Engl J Med 2017; 376: http://www.nejm.org/doi/full/10.1056/NEJMicm1405867
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#创伤性#
61
#创伤#
50
学习,感谢分享!
84