NEJM:急性跟腱断裂的非手术或手术治疗效果比较
2022-04-15 MedSci原创 MedSci原创
在跟腱断裂的患者中,手术(开放修复或微创手术)治疗在12个月的疗效并不比非手术治疗获得更好的结局。
跟腱是足踝后部人体最强大的肌腱,能承受很大的张力,除个别疾病和特殊的动作外,在日常生活中很难发生断裂。跟腱的功能是负责踝关节的跖屈,对于行走等日常生活得动作的完成起重要的作用。跟腱断裂发生的高危人群是学生运动员和演员,近年群众体育的广泛开展和运动水平的不断提高,跟腱断裂的发病率逐年提高。除少数跟腱原位外伤导致的开放性跟腱断裂外,大部分跟腱断裂是由间接外力引发。部分跟腱断裂的患者在发生跟腱断裂前都有跟腱相关的慢性疾病。跟腱断裂亦高发于仅于闲暇日或休息日进行较大运动量体育活动的人。在四季分明的区域跟腱断裂好发于开春及初秋。
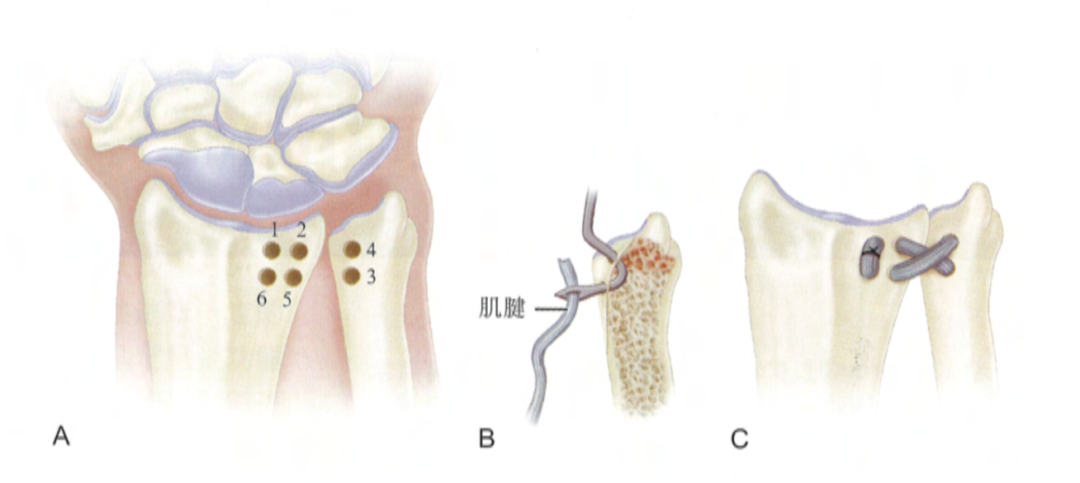
急性跟腱断裂最佳治疗方案在临床上存在较多争议。有研究发现,急性跟腱锻炼通过保守石膏制动固定或者手术修复等均可以取得愈合,并且功能基本类似;两者的差别在于,前者有更高的再断裂率,后者有更高的并发症发生率。
急性跟腱断裂是最常见的肌肉骨骼损伤之一,每年每10万人发生5至50起事件,并可能导致严重残疾。这种损伤在老年人、更积极的生活方式和男性中更为常见,在过去几十年发病率一直在上升。急性跟腱断裂的手术修复,无论是开放修复还是微创修复,是否比非手术治疗容易获得更好的结果尚未明确。

近日,顶级医学期刊NEJM上发表了一篇研究文章,研究人员进行了一项多中心、随机、对照试验,比较了在四个试验中心就诊的急性跟腱断裂成人患者的非手术治疗、开放修复和微创手术的疗效。该研究的主要结果是从基线开始到12个月时跟腱总断裂评分(评分范围从0到100,评分越高表明健康状况越好)变化。该研究的次要结局包括肌腱再次断裂的发生率。

该研究共有554例患者进行随机分组,526例患者纳入最终分析。跟腱总断裂评分的平均变化在非手术组为-17.0分,开放修复组为-16.0分,微创手术组为-14.7分(P=0.57)。
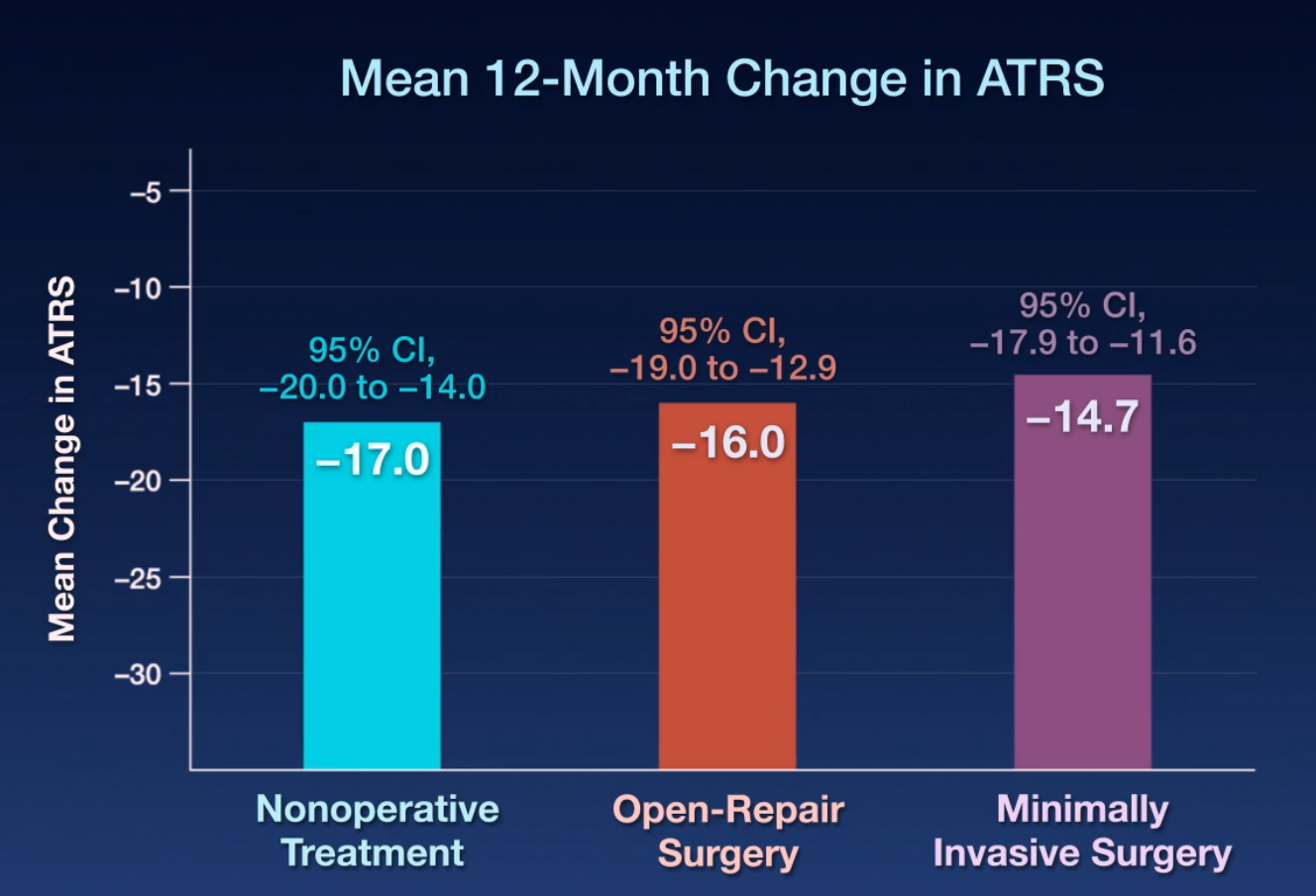
两两比较没有提供组间差异的证据。从基线开始,三组患者的身体机能和患者报告的身体机能的变化是相似的。非手术组肌腱再断裂的次数(6.2%)高于开放修复组或微创手术组(各为0.6%)。微创手术组有9例神经损伤(5.2%),开放修复组有5例神经损伤(2.8%),非手术组有1例神经损伤(0.6%)。
由此可见,在跟腱断裂的患者中,手术(开放修复或微创手术)治疗在12个月的疗效并不比非手术治疗获得更好的结局。
原始出处:
Ståle B. Myhrvold.et al.Nonoperative or Surgical Treatment of Acute Achilles’ Tendon Rupture.NEJM.2022.https://www.nejm.org/doi/full/10.1056/NEJMoa2108447
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#治疗效果#
102
#跟腱断裂#
95
#急性跟腱断裂#
96
#手术治疗#
105
这里最主要思考,这样的研究为什么能发表在顶级期刊#新英格兰杂志#上??
177
NEJM上果然牛,感谢梅斯更新及时
84