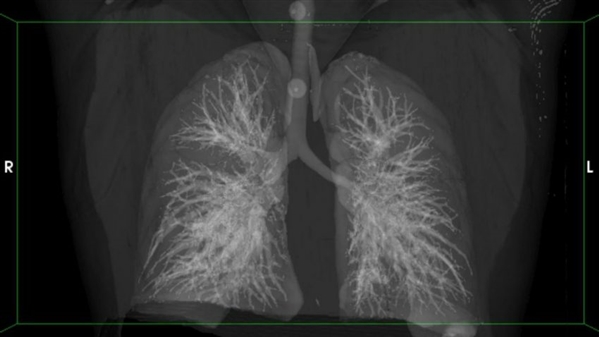
Cell:揭示抗体在控制肺结核中的作用
2016-10-06 佚名 生物谷
在一项新的研究中,来自由美国麻省总医院、麻省理工学院和哈佛大学联合组建的拉根研究所(Ragon Institute)的研究人员发现证据证实抗体保护可能有助控制导致肺结核(TB)的细菌感染。他们描述了靶向活动性肺结核患者和潜伏性肺结核患者体内的肺结核菌的抗体在结构和功能上存在的一致性差异,其中潜伏性肺结核患者并不产生症状,也不能够传播疾病。这些发现可能导致更好的方法来区分活动性肺结核和潜伏性肺结

论文共同第一作者、拉根研究所研究员Lenette Lu博士说,“到2030年终结肺结核是世界卫生组织新实施的可持续发展目标之一。一种更加有效地抵抗肺结核的疫苗可能能够实质上促进这一目标实现,影响着全世界每3名肺结核患者当中的将近1名和解决HIV感染者的主要杀手。”
当前唯一获得的抵抗肺结核菌感染的预防措施---BCG疫苗---自从二十世纪二十年代以来就被人们使用;但是它抵抗肺结核的有效性总是无法确定的。BCG疫苗被认为通过激活细胞免疫反应来发挥作用,这种细胞免疫反应是通过肺结核菌直接感染的T细胞和巨噬细胞等特定的免疫细胞来执行的。之前对抗体在针对肺结核菌的免疫反应中可能发挥的作用的研究产生相互冲突的结果,但是在这项新的研究中,在麻省总医院医学系研究员Galit Alter博士和哈佛陈曾熙公共卫生学院(Harvard T.H.Chan School of Public Health)研究员Sarah Fortune博士的领导下,研究人员采用了一种新的方法。
除了结合到靶病原体和对它们进行标记以便被免疫系统破坏之外,抗体也直接通过结合一种被称作Fc受体的细胞表面蛋白来激活先天免疫系统中杀死病原体的细胞。研究人员分析了来自22名潜伏性肺结核患者和20名活动性肺结核患者的肺结核特异性抗体的70种不同的与Fc介导的抗体功能相关联的特征。他们首先鉴定出区分这两组参与者抗体的9种特征,而进一步的研究鉴定出最好地区分这两组参与者的生物标志物。
一种Fc介导的免疫功能的关键性调节物是结合到抗体上的被称作聚糖(glycan)的化合物,其中聚糖是由糖分子组成的;糖基化模式上的显著差异被发现明确地区分潜伏性肺结核抗体和活动性肺结核抗体。为了证实在初始的来自南非的这组参与者体内获得的这些结果,研究人员对来自美国德克萨斯州和墨西哥的20人---10人患上潜伏性肺结核,10人患上活动性肺结核---的抗体开展类似的分析,并且取得相同的结果。进一步的实验揭示出将潜伏性肺结核抗体加入到被肺结核菌感染的人巨噬细胞中不仅会增加几种抗微生物过程的激活,而且也会降低肺结核菌的存活。
论文共同第一作者Amy Chung博士解释道,“这是肺结核的一个全新的免疫研究领域,这是因为这些抗体并不只是识别这种肺结核菌感染,它们也招募免疫细胞来靶向这种感染。遭遇潜伏性肺结核菌感染的人们因某种原因患有非活动性的疾病,如果抗体在这种感染中发挥着作用的话,那么它们使用的机制可能被用于未来的疫苗开发。”
Alter补充道,“这些发现的诊断潜力不应当被忽视。检测肺结核特异性抗体的Fc相关性修饰可能很容易被转化为一种快速的廉价的即时诊断方法从而可能产生巨大的健康影响,特别是对地球上发生肺结核流行病的那些地方。”
Lenette L. Lu11, Amy W. Chung11, Tracy R. Rosebrock11, Musie Ghebremichael, Wen Han Yu, Patricia S. Grace, Matthew K. Schoen, Fikadu Tafesse, Constance Martin, Vivian Leung, Alison E. Mahan, Magdalena Sips, Manu P. Kumar, Jacquelynne Tedesco, Hannah Robinson, Elizabeth Tkachenko, Monia Draghi, Katherine J. Freedberg, Hendrik Streeck, Todd J. Suscovich, Douglas A. Lauffenburger, Blanca I. Restrepo, Cheryl Day, Sarah M. Fortune, Galit Alter.A Functional Role for Antibodies in Tuberculosis.Cell.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
57
#Cell#
58
继续关注!
84
谢谢分享!
92
#结核#
0