Cancer Cell:癌细胞如何在没有葡萄糖的条件下继续增殖扩张?
2016-08-10 佚名 生物谷
肿瘤细胞最主要的目标就是生存,其甚至不惜破坏其所依附的有机体的健康也要达到生存的目的;为了生存肿瘤细胞会练就许多健康细胞没有的本领,包括在葡萄糖水平极低的情况下继续保持生长势头,而这或许就是常用的抗血管生成因子难以消除癌症的主要原因,肿瘤细胞通常会通过妨碍提供常规的营养物质和葡萄糖的血管的发育来影响机体健康,如今来自西班牙国立癌症研究中心(CNIO)的研究人员通过研究鉴别出了一种关键的生化机制,该
肿瘤细胞最主要的目标就是生存,其甚至不惜破坏其所依附的有机体的健康也要达到生存的目的;为了生存肿瘤细胞会练就许多健康细胞没有的本领,包括在葡萄糖水平极低的情况下继续保持生长势头,而这或许就是常用的抗血管生成因子难以消除癌症的主要原因,肿瘤细胞通常会通过妨碍提供常规的营养物质和葡萄糖的血管的发育来影响机体健康,如今来自西班牙国立癌症研究中心(CNIO)的研究人员通过研究鉴别出了一种关键的生化机制,该机制可以使得癌细胞在没有葡萄糖的情况下继续生存,相关研究刊登于国际杂志Cancer Cell上。
文章中,研究者发现了一类扮演开关作用的特殊蛋白,即当葡萄糖可用时,肿瘤细胞就会利用特殊的生化路径来生存并且继续增殖,而当环境中没有葡萄糖时,这种蛋白开关就会诱发一种不同的通路来完成相同的目标,这就称之为肿瘤细胞特殊的生存模式。研究者Nabil Djouder解释道,肿瘤细胞非常聪明,当对其生长和增殖必要的一扇门关闭时,它们总会打开另外一扇门来适应任何压力并且不断生长,这就是为何癌细胞会产生高度复杂的机制来学会生存以及科学家们很难对付癌症的原因。
很长一段时间以来,科学家们非常疑惑肿瘤细胞到底是如何设法在大规模的肿瘤内部(肿瘤内部中央位置)生存的,因为肿瘤组织中心几乎没有任何血管提供营养物质,研究者目前迫切希望理解癌细胞对抗血管生成因子产生耐药性的机制,抗血管生成因子是近年来常用的一种广泛的抗癌药物,其作用效力基于抑制对肿瘤提供营养物质的血管网络,从而使得癌细胞因得不到营养物质而死亡。
不管是否为癌细胞,在细胞中都会发生任何事情, 而这基于细胞中的一系列生化反应,即通过添加特殊分子来对蛋白质进行修饰,而且这种改变还会诱导其它蛋白的改变,这就好比携带了多个能够连接/断开的开关组成的回路一样,研究者Djouder及其同事就在文章中鉴别出了这种开关系统,其可以帮助细胞检测环境中是否存在葡萄糖,并且帮助细胞决定它们应当遵循什么样的生化路径来按成最终生存的目的。
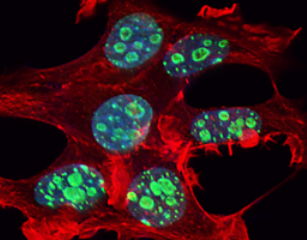
这种复杂的系统由三种蛋白组成:URI蛋白(扮演开关作用)、OGT和c-Myc;c-Myc是一种熟知的癌基因,其可以促进细胞增殖和生存,然而研究者发现c-Myc蛋白的水平对于癌细胞生存的重要性要远远高于营养物质的压力。研究者指出,URI蛋白可以控制OGT的活性,而OGT可以感知并且利用葡萄糖来控制c-Myc的水平。当存在葡萄糖时,OGT会利用葡萄糖来稳定c-Myc的水平;反之,细胞则会面临葡萄糖短缺的状况,URI则会变成OGT的潜在抑制子,并且抑制OGT的活性,从而降低细胞对葡萄糖的消耗,最终导致c-Myc降解;在葡萄糖缺失的情况下,细胞的生存依赖于具有癌基因活性的URI蛋白。
这项研究中,研究者阐明了一种重要的葡萄糖感知机制,即URI蛋白可以扮演控制OGT和c-Myc活性的“变阻器”,其会被赋予选择性的特性来促进癌细胞对多种代谢压力产生耐受,并且在由环境改变引发的选择性压力环境中继续生存下去。这种新型机制对于研究肿瘤形成非常关键,或许可以帮助研究者解释葡萄糖缺失时癌细胞如何能够继续扩张。
本文研究结果对于进行实际临床应用或许还有一段距离,比如截止到目前为止研究者还不能成功阻断URI蛋白的活性,而且研究者还不能完全解析URI蛋白的功能,后期研究者表示他们还将通过更为深入的研究来深入剖析URI蛋白的功能以及其同癌症生存的关系。
原始出处
Stefan Burén, Ana L. Gomes, Ana Teijeiro, Mohamad-Ali Fawal, Mahmut Yilmaz, Krishna S. Tummala, Manuel Perez, Manuel Rodriguez-Justo, Ramón Campos-Olivas, Diego Megías, Nabil Djouder.Regulation of OGT by URI in Response to Glucose Confers c-MYC-Dependent Survival Mechanisms.Cancer Cell.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
40
#Cell#
48
#扩张#
42
#cancer cell#
51
有可能最终改变世界的研究
97
#癌细胞#
107
内容新颖
78