一个蛋白竟可同时影响乳腺癌和淋巴癌的形成与扩散
2016-08-18 佚名 药明康德
近日,来自新加坡科技研究局(A*STAR)和新加坡国立大学的科学家们发表了对致癌基因EZH2的最新研究,他们首次发现EZH2分别在乳腺癌和淋巴癌形成和扩散中的新机制。这些新发现有望带来治疗这两种癌症的新药物。EZH2基因已知与多种癌症相关,研究发现在乳腺、膀胱、前列腺等多种肿瘤内,EZH2的表达量上升。EZH2编码的蛋白是组蛋白赖氨酸甲基转移酶,在正常情况下它是多梳蛋白复合物PRC2的成员和其主要
近日,来自新加坡科技研究局(A*STAR)和新加坡国立大学的科学家们发表了对致癌基因EZH2的最新研究,他们首次发现EZH2分别在乳腺癌和淋巴癌形成和扩散中的新机制。这些新发现有望带来治疗这两种癌症的新药物。
EZH2基因已知与多种癌症相关,研究发现在乳腺、膀胱、前列腺等多种肿瘤内,EZH2的表达量上升。EZH2编码的蛋白是组蛋白赖氨酸甲基转移酶,在正常情况下它是多梳蛋白复合物PRC2的成员和其主要催化部分,在胚胎发育过程中起到调控基因表达的重要作用。然而,过量表达的EZH2在癌症中的作用却不太为人所知。
在对于乳腺癌的研究中,研究人员惊异地发现,在肿瘤形成早期,含有EZH2的PRC2复合物对于肿瘤的生长有抑制作用。那么是什么导致了EZH2从人体的保护者变成癌症的帮凶呢?原来,当肿瘤生长到一定的程度时,由于血液供应不足,肿瘤内部的癌细胞会处于缺氧状态。缺氧状态下的癌细胞激活了缺氧因子HIF1a的表达,HIF1a使得EZH2脱离PRC2复合物,并与另一个致癌蛋白FoxM1结合,导致肿瘤的迅速生长和扩散。重要的是,这一过程与EZH2本身的催化功能无关。同时,研究人员还注意到该现象在三阴性乳腺癌中更常见。三阴性乳腺癌目前缺乏有效的治疗手段,因此这项发现有可能带来针对三阴性乳腺癌的新药。
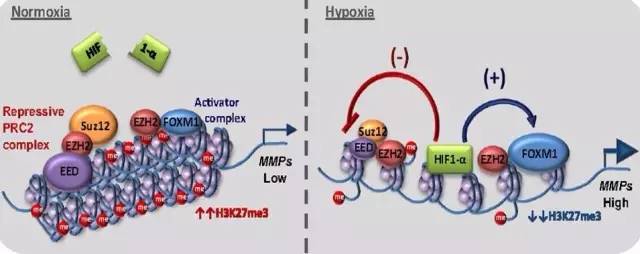
▲EZH2的乳腺癌致癌机理(图片来源:PNAS)
在另一项研究中,新加坡科学家针对的是一种较为罕见,但在亚洲人群中更常见的自然杀伤/T细胞淋巴癌。在这种癌症中,EZH2的功能受到蛋白激酶JAK3的调控。EZH2被JAK3磷酸化后,同样能够脱离PRC2复合物,然后其非催化功能加快了癌细胞的生长。在自然杀伤/T细胞淋巴癌中,JAK3的突变或激活非常常见。当使用药物抑制JAK3的活性后,EZH2的磷酸化程度降低,使得癌细胞生长变缓。
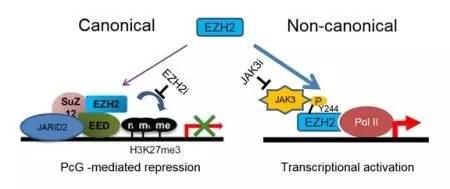
▲EZH2的淋巴癌致癌机理(图片来源:A*STAR)
这两项研究发现在不同的癌症中,EZH2却有相似的致癌机制。更重要的是,该机制并非通过EZH2的传统催化功能实现,当EZH2脱离了PRC2复合物后,其非催化功能发生作用以促进癌细胞生长。研究的参与者Wee Joo Chng教授表示:“这些研究改变了我们对于EZH2致癌机制的传统认识。当我们开发针对EZH2的新药时需要仔细辨别在某种特定的癌症中究竟是它的催化功能还是非催化功能在起作用,仅仅抑制EZH2的催化功能反而可能加速癌症病情的发展,因此我们也需要寻找其非催化功能的抑制剂。”
新加坡基因研究院执行主任Huck Hui Ng教授评论道:“这两项研究突出了科研人员合作的重要性。随着对EZH2在不同癌症中不同功能的深入研究,将有望为我们带来全新的药物。”我们希望针对EZH2不同功能的不同抑制剂能够早日被发现,从而能够为癌症患者,尤其是三阴性乳腺癌和淋巴癌等较难治疗的癌症带来福音。
参考资料:
1. A*STAR Release: Singapore Scientists Discover New Pathways Leading To Cancer Progression
2. HIFI-α activation underlies a functional switch in the paradoxical role of EZH2/PRC2 in breast cancer
3. EZH2 phosphorylation by JAK3 mediates a switch to non-canonical function in natural killer/T-cell lymphoma.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













这篇资讯写的真好,带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
81
学习了,很好的知识!
84
值得学习
87
#淋巴癌#
58
学习了,赞一个!
90
学习了,赞一个!
79