JBJS:固定衬垫全踝关节置换术后疗效良好
2013-08-01 第五十七回 dxy
最近一些前瞻性对照研究以及荟萃分析结果显示现代全踝关节置换(TAA)治疗有症状的终末期踝关节炎的疗效与踝关节融合相当。现代TAA系统拥有固定衬垫和活动衬垫两种设计形式。目前世界范围内使用最广泛的是活动衬垫的三体式踝关节假体系统,但在美国则主要是固定衬垫的双体式假体系统。 Salto Talaris全踝关节假体系统是一种基于Salto活动衬垫的新型TAA假体。这种假体系统是固定衬垫型假体,但术中却
最近一些前瞻性对照研究以及荟萃分析结果显示现代全踝关节置换(TAA)治疗有症状的终末期踝关节炎的疗效与踝关节融合相当。现代TAA系统拥有固定衬垫和活动衬垫两种设计形式。目前世界范围内使用最广泛的是活动衬垫的三体式踝关节假体系统,但在美国则主要是固定衬垫的双体式假体系统。
Salto Talaris全踝关节假体系统是一种基于Salto活动衬垫的新型TAA假体。这种假体系统是固定衬垫型假体,但术中却是使用可旋转的胫骨侧假体试模,通过试模的旋转自动获得正确的踝关节力线,满意后植入最终假体,其胫骨侧聚乙烯衬垫固定于金属假体上,不能发生任何旋转及平行移位等活动。
美国杜克大学医学中心的Schweitzer Jr KM等对67例接受Salto Talaris 固定衬垫式TAA假体系统治疗的患者进行了最少2年的随访研究,根据相关研究结果他们认为该假体系统能有效缓解疼痛,改善关节功能并提高生活质量。相关研究结果发表于最新一期JBJS[Am]上。
Schweitzer Jr KM等在2007年6月至2009年10月之间于一家三级医疗中心以Salto Talaris固定衬垫式TAA假体系统对67例终末期踝关节炎患者进行了关节置换治疗。所有患者均经长期保守治疗无效,且无活动性感染、严重外周血管病变、以及未得到控制的糖尿病等。但排除骨量不足或踝关节冠状面上畸形超过20o的患者。术后随访时间不足2年的8例患者亦不纳入研究分析。
结果总共67例患者(男性18例,女性49例)术后平均随访2.81年(范围:2.00-4.46 年)。本组患者平均年龄63岁(范围:34-86岁)。51例(76%)诊断为创伤性关节炎,11例骨关节炎,3例类风湿性关节炎,1例牛皮癣性关节炎,1例血色病性关节病。平均BMI为29.3(范围:20.3-42.6)。3例病人患2型糖尿病,但控制良好;本组无1型糖尿病患者。5例患者正服用至少一种免疫抑制剂。
所有手术均以相同的技术按产品操作手册进行,术后患肢均以石膏固定制动。术后第2天开始逐步进行患肢不负重活动及理疗。术后3周取除原石膏更换为短腿石膏或支具继续固定患肢并不负重活动3周。术后6周至3月由患者根据自身感觉情况进行主动功能锻炼,并逐步进行功能锻炼。
所有病例均于术后6周、3月、6月、1年,此后每年1次定期进行临床及影像学随访检查。每次随访时均要求患者完成标准化问卷表,并分别于术前及术后1、2年时完成标准化功能评估。
临床及影像学评估方法包括:
1、详细的查体以及踝关节负重位X片(前后位、侧位、踝穴位);
2、完成标准化评估,包括视觉模拟疼痛评分(VAS)、美国足踝外科医师学会(AOFAS)后足评分、SF-36健康评分量表、简明骨胳肌肉评估(SMFA)问卷等;
3、在前述随访时间点时,针对每例患者完成标准化的踝关节功能测试,包括:坐站测试、计时起走测试、平均步速测定等;并完成足踝功能障碍指数(FADI)问卷;
研究结果如下:
1、2/3的病例(45/67)于TAA手术同时进行了至少一种其它手术操作,其中主要为深层三角韧带松解、取除原内固定物、以及腓肠肌松解;6例患者进行了预防性内踝固定;另有2例术中内/外踝骨折,均予以内固定处理;
2、术后平均住院日为1.5天(范围:1-5天),44例(66%)患者术后第一天出院;1例患者术后发生双侧肺动脉栓塞,经抗凝治疗好转;
3、8例患者(12%)术后再次接受手术处理,主要是因关节碰撞行骨赘切除及关节清理;
4、按改良Glazebrook等的TAA并发症分级标准,共15例患者出现23项并发症,其中7例(9项)接受再次手术,包括2例患者出现TAA假体无菌性松动。本组无深部感染病例。术后平均2.81年随访时,本组假体总生存率为96%;
5、临床评估结果显示:术后VAS疼痛评分、SF-36总体评分及次级评分结果、SMFA功能及其它指标评分、平均AOFAS后足总体评分和疼痛以及功能评分均较术前显著提高;
6、影像学评估结果显示:术前术后冠状面上内翻角分别为2.2o(范围:16.4o内翻-15.5o外翻)和0.2o(范围:5.1o内翻-6.1o外翻),75%的病例冠状面上力线位于2o内翻-2o外翻之间;3例患者出现胫骨侧假体松动;分别有26例及10例患者出现胫骨侧及距骨侧假体周围透亮线,但除前述3例失败病例外,无一例出现进展或症状;
7、功能评估结果显示:坐站试验由术前平均18.1 ± 6.8秒显著提高至术后1年和2年时的15.2 ± 4.2秒及12.7 ± 3.1秒;计时起走试验由术前平均0.86 ± 0.28 m/s提高至术后1年和2年的1.15 ± 0.25 m/s以及1.21 ± 0.17 m/s;平均步速和FADI评分同样均有显著提高。
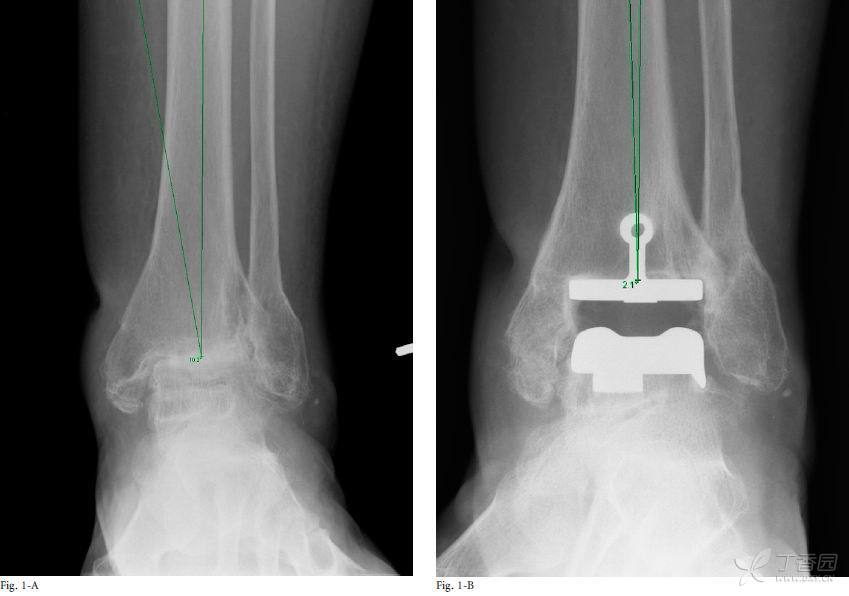
图1 术前前后位X片显示踝关节冠状面上外翻10.2o,术后3年前后X片上显示该外翻角矫正至2.1o内翻
表I TAA手术同时进行的手术操作情况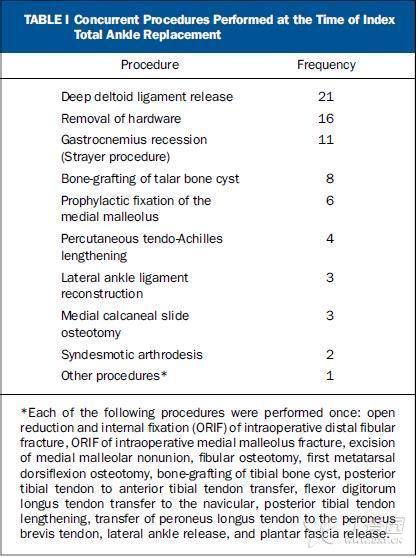
表II TAA术后再手术情况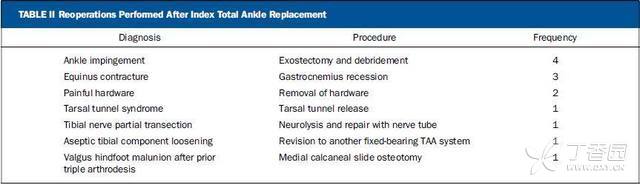
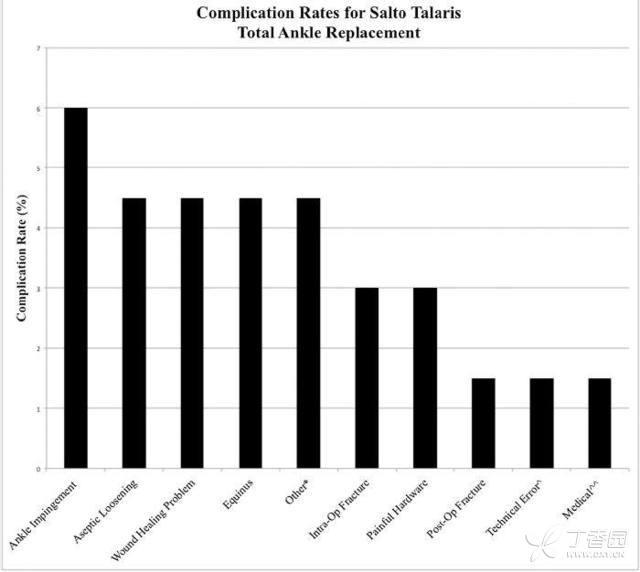
图2 按改良Glazebrook标准对TAA术后并发症的分级情况。 * “Other”指三例踝管综合征;^“Technical error”指胫神经部分切断;^^“Medical complication”指发生双侧肺动脉栓塞患者;Intra-Op = intraoperative(术中), Post-Op = postoperativ e(术后)

图3 术后1年(图3-A)以及术后2年(图3-B)患肢负重位踝关节侧位X片显示胫骨假体背侧进展性透亮线。该患者行走时有不适症状并最终出现关节疼痛及活动障碍,随后该病例以固定衬垫TAA假体系统予以翻修
表III 本组病例疗效情况
表IV 踝关节功能评估结果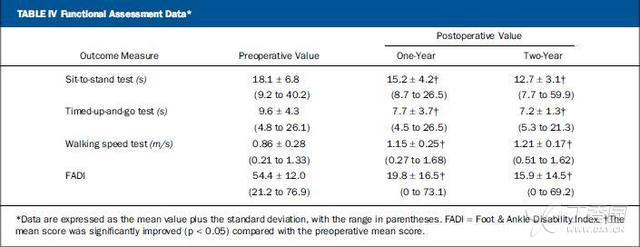
Schweitzer Jr KM等认为,该研究是截至目前为止样本量最大且随访时间较长的有关Salto Talaris TAA系统的研究,其结果显示终末期踝关节炎患者采用该假体置换术后患肢疼痛明显缓解,肢体功能恢复良好。但仍需要进一步的研究探讨可能导致术后失败的相关因素,并有必要与固定衬垫式的假体系统进行前瞻性的比较研究以了解衬垫类型是否与TAA术后疗效相关。

Schweitzer KM, Adams SB, Viens NA, Queen RM, Easley ME, Deorio JK, Nunley JA.Early prospective clinical results of a modern fixed-bearing total ankle arthroplasty.J Bone Joint Surg Am. 2013 Jun 5;95(11):1002-11. doi: 10.2106/JBJS.L.00555.
- PMID:
- 23780538
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#置换#
65
#关节置换术#
90
#踝关节#
71
#置换术#
84
#JBJS#
62