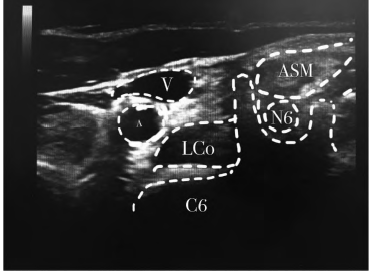
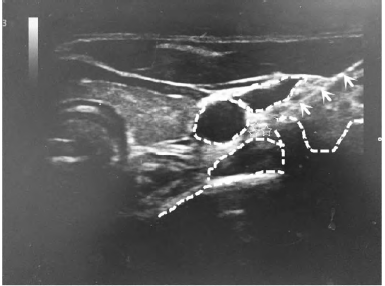
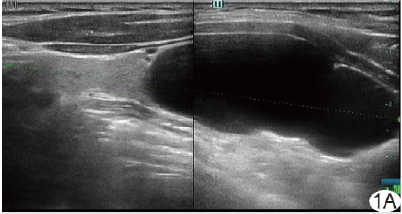
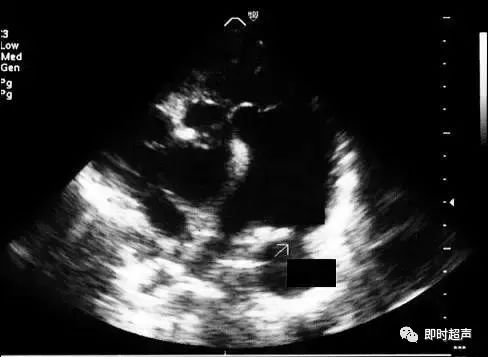
超声引导下星状神经节阻滞治疗头颈部带状疱疹爆发痛1例
2019-05-22 周红梅 张建楠 裴燕芳 中国医药导报
患者,女,64岁,因“左侧耳垂、枕部疼痛4d伴左颈部红斑、疱疹1d”于2017年6月16日入院。既往有高血压病史,平时口服“氢氯噻嗪片”“螺内酯”“乐卡地平”,血压控制尚可。患者入院前3d因耳垂、枕部阵发性刀绞般疼痛来我科门诊就诊,当时行颈椎间盘CT示无明显异常,予加巴喷丁胶囊0.3g口服,3次/d,洛芬待因片200mg口服,3次/d,对症治疗,嘱门诊随诊。


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#超声引#
69
#超声引导#
75
#头颈部#
74
#疱疹#
0
#颈部#
76