Hepatology:TIPS治疗非肝硬化性门静脉高压症患者的并发症是安全有效的
2016-07-15 Seven L 译 MedSci原创
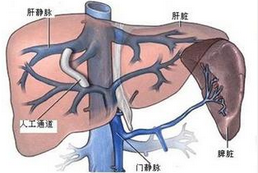
近期发表在Hepatology的研究称,对于肾功能正常、无严重肝外并发症的特发性非肝硬化性门静脉高压症(INCPH)患者,经颈静脉肝内门体分流术(TIPS)治疗门脉高压(PHT)并发症是安全和有效的。研究人员掉2000-2014年间的41名患者进行了回顾性研究。TIPS的适应证为:复发性静脉曲张出血(n = 25)和难治性腹水(n = 16)。根据患者是否存在肝外合并症(包括血液系统、血栓、肿瘤、
近期发表在Hepatology的研究称,对于肾功能正常、无严重肝外并发症的特发性非肝硬化性门静脉高压症(INCPH)患者,经颈静脉肝内门体分流术(TIPS)治疗门脉高压(PHT)并发症是安全和有效的。
研究人员对2000-2014年间的41名患者进行了回顾性研究。TIPS的适应证为:复发性静脉曲张出血(n = 25)和难治性腹水(n = 16)。根据患者是否存在肝外合并症(包括血液系统、血栓、肿瘤、免疫毒素等)进行分组:存在(n = 27)或不存在(n = 14)。平均随访27个月。
在随访中,25例患者中有7名出现了食管静脉曲张破裂出血,包括3例早期的支架血栓形成。41名患者中有14名出现了TIPS后明显的肝性脑病。4名腹腔积血患者完成了TIPS,其中1名是致命的。
总体而言,共发生了11例死亡。死亡与以下因素有关:腹水(P = .04)、血清肌酐(P = .005)、进行TIPS时存在明显的并发症(P = .01)。此外,死亡更多见于重要合并症和肌酐水平≥100 µmol/L的患者(P < .001)。
研究人员写道,这是目前关于TIPS治疗INCPH患者PHT并发症的最大的研究。结果表明,对于肾功能正常、无严重肝外并发症的INCPH患者,选择TIPS治疗PHT并发症是安全有效的。
原始出处:
Bissonnette J, et al.Role of the transjugular intrahepatic portosystemic shunt in the management of severe complications of portal hypertension in idiopathic noncirrhotic portal hypertension. Hepatology. 2016;doi:10.1002/hep.28547.
TIPS safe, effective in patients with idiopathic noncirrhotic portal hypertension.Healio.July 14, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#静脉#
127
#TIPS#
99
#门静脉高压症#
91
#并发#
80
好文章
150
#iPS#
84
#EPA#
80
#门静脉#
133
#硬化性#
73