拜耳放弃研发P2X3受体拮抗剂eliapixant
2022-02-05 Allan MedSci原创
该计划暂停的消息是在 FDA 为默克公司的口服 P2X3 受体拮抗剂 gefapixant 发出完整的回复信之后发布的,该公司正在寻求 FDA 批准 gefapixant 用于治疗慢性咳嗽。
P2X3 受体是位于初级传入神经元上的ATP离子门控通道。从气道中受损或发炎的组织释放的ATP作用于初级传入神经元的 P2X3 受体,触发去极化和动作电位,这些电位被集中传播并被解释为咳嗽的冲动(图1)。有大量的临床前和临床证据支持 P2X3 受体在咳嗽反射超敏反应中导致慢性咳嗽的作用。
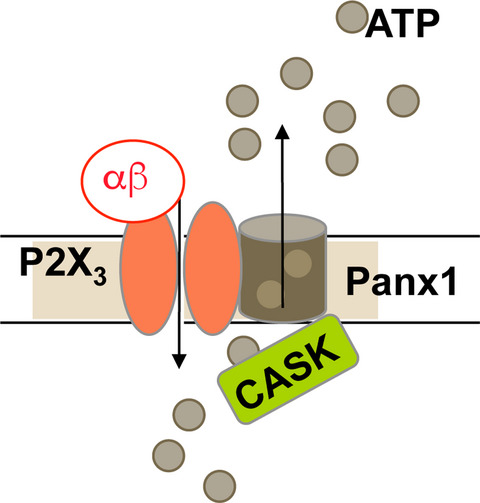
图1.P2X3 受体参与咳嗽的病理形成过程
拜耳本周五表示,它正在结束实验性 P2X3 受体拮抗剂 eliapixant 的开发,该公司正在评估 eliapixant 治疗子宫内膜异位症、难治性慢性咳嗽、膀胱过度活动症和糖尿病性神经性疼痛等适应症的可行性。
拜耳去年 9 月报告的结果显示,每日两次口服 eliapixant 达到了针对难治性慢性咳嗽患者的 IIb 期 PAGANINI 研究的主要终点,与安慰剂相比,eliapixant 组患者的 24 小时咳嗽计数减少了 27%。当时,该公司表示,eliapixant 似乎具有积极的收益-风险特征,大多数不良事件 (AE) 被认为是轻度或中度的,尽管在接受 eliapixant 治疗的患者中有 8% 的患者因 AE 而退出试验,而接受最高剂量 eliapixant 的人中有 24% 出现了与味觉相关的副作用。
该计划暂停的消息是在 FDA 为默克公司的口服 P2X3 受体拮抗剂 gefapixant 发出完整的回复信之后发布的,该公司正在寻求 FDA 批准 gefapixant 用于治疗慢性咳嗽。
默克表示,它仍致力于推进 gefapixant,该药物最近在日本以 Lyfnua 的名称获批,用于治疗患有难治性或不明原因慢性咳嗽的成人。
慢性咳嗽是指咳嗽持续时间超过8周以上。对于临床医生而言,慢性咳嗽经过胸部X线检查,没有发现明确的肺部病变所能解释咳嗽病因时,称为不明原因的慢性咳嗽。这些常见的不明原因的慢性咳嗽病因,主要包括咳嗽变异性哮喘、上气道咳嗽综合征、胃食管反流性咳嗽、嗜酸粒细胞性支气管炎、变应性咳嗽。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#研发#
95
#拜耳#
98
#拮抗剂#
95
学习了
127
不赖1
112
学习了
101