The Lancet Oncology:Avelumab用于转移性或局部晚期实体瘤
2017-04-01 MedSci MedSci原创
Avelumab用于晚期实体瘤安全有效
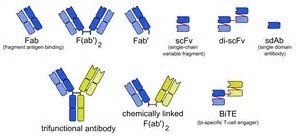
Avelumab (MSB0010718C)是一种人源IgG1单克隆PD-L1抗体,研究人员就其对于实体瘤患者的安全性以及药代动力学性质进行评估,结果发表于近日的The Lancet Oncology。
18岁以上的转移或局部晚期实体肿瘤患者参与了试验,研究使用4个不同的Avelumab剂量(1、3、10、20mg/kg),每2周注射一次。主要终点是使用Avelumab 3周的剂量-毒性关系,次要终点是药物安全性、药效以及药代动力学。
研究招募了53名病人(4人接受1mg/kg 、13人接受mg/kg 、15人接受10mg/kg、 21人接受20mg/kg),其中18名患者接受剂量-毒性分析试验(3人接受1mg/kg、3人接受3mg/kg、6人接受10mg/kg、6人接受10mg/kg)。研究中只有20mg/kg剂量组出现的毒性;最常见的不良事件为疲劳(40%)、流感样症状(21%)、发热(15%)、寒冷(11%);3级以上的不良事件报告9起(17%):3起自身免疫失调、2起血肌酸磷酸激酶、2起天冬氨酸转氨酸升高。8%患者治疗效果明显,57%患者病情得到控制;药物半衰期为95-99小时(10-20mg/kg组);有2名患者体内检测到了抗药抗体;试验中没有患者死亡。
研究者认为Avelumab最大可耐受剂量可以达到20mg/kg,综合分析试验结果,将采用每2周10mg/kg的剂量用于后续的研发。
原文出处:
Christopher R Heery et al. Avelumab for patients with previously treated metastatic or recurrent non-small-cell lung cancer (JAVELIN Solid Tumor): dose-expansion cohort of a multicentre, open-label, phase 1b trial. The Lancet Oncology. 2017 Mar 31
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Oncol#
61
#Lancet#
53
#局部晚期#
52
#mAb#
62
#Oncology#
53
#avelumab#
46
#转移性#
49
#局部#
58
#晚期实体瘤#
72