JAHA:房颤对Takotsubo综合征患者结局的影响
2021-07-28 MedSci原创 MedSci原创
房颤(AF)是导致死亡的主要危险因素。尚未在大型患者队列中探究AF在Takotsubo综合征(TTS)患者中的患病率、临床相关性以及预后影响。
房颤(AF)是导致死亡的主要危险因素。尚未在大型患者队列中探究AF在Takotsubo综合征(TTS)患者中的患病率、临床相关性以及预后影响。
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究旨在调查TTS患者AF的患病率、临床相关性以及预后影响。TTS患者来自国际Takotsubo注册中心,这是一个跨国网络,包含了欧洲和美国的26个参与中心。根据受试者入院时是否存在AF将患者分为两类。

在1584名TTS患者中,112名(7.1%)TTS患者伴有AF。与非AF组相比,AF组的平均年龄较高(P<0.001),且女性较少(P=0.046)。AF组左心室射血分数显著降低(P=0.001),心源性休克更常见(P<0.001)。房颤组的住院死亡率(P<0.001)和长期死亡率(P<0.001)均较高。
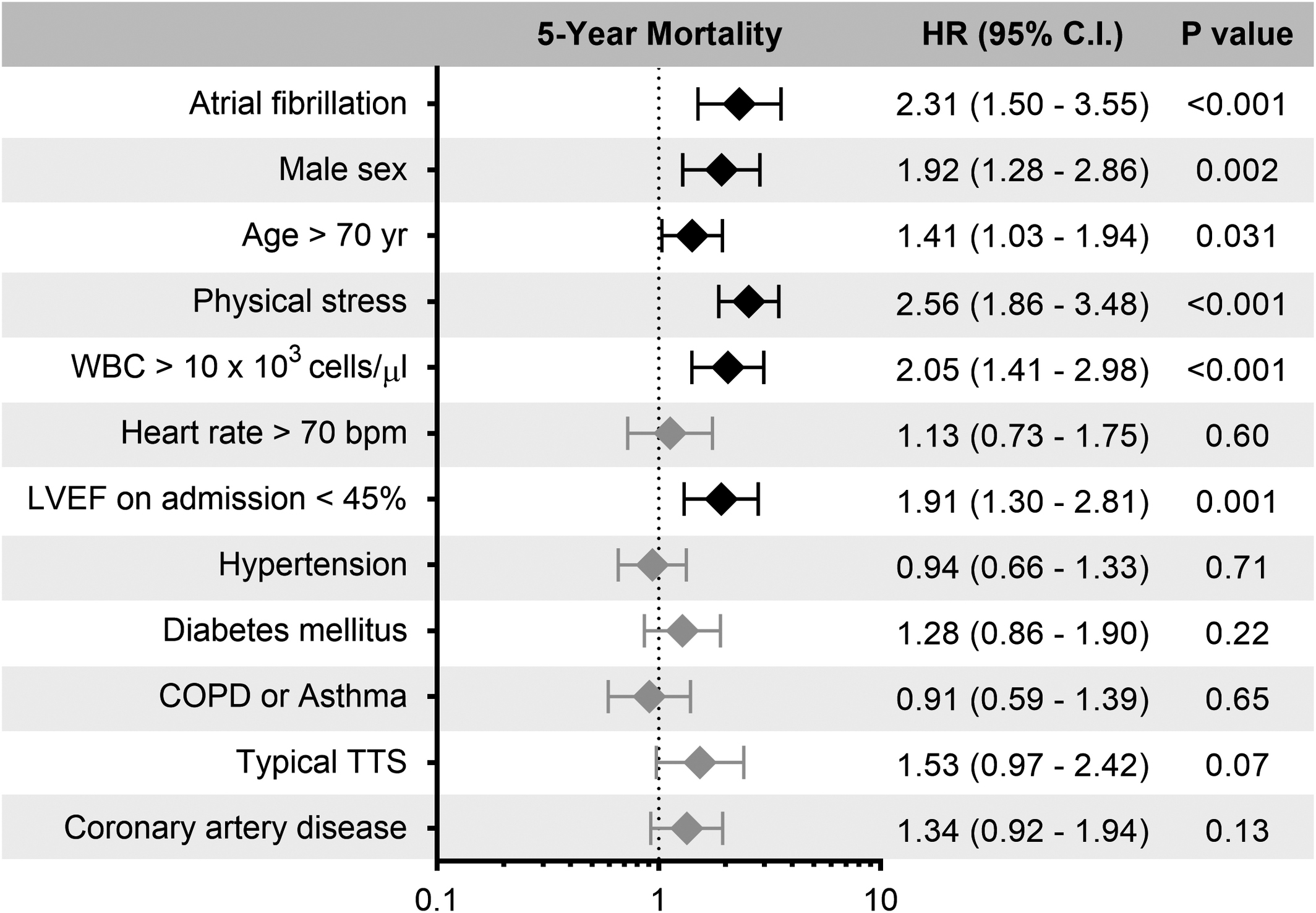
多变量COX回归分析结果
多变量Cox回归分析发现AF与较高的长期死亡率独立相关(风险比为2.31;95%CI为1.50-3.55;P<0.001)。在入院时伴有AF的患者中,42%的患者在发生急性TTS事件之前没有AF病史,与有AF病史的患者相比,这些患者的院内和长期预后相当。
由此可见,在TTS患者中,入院时伴有AF与院内和长期死亡率增加显著相关。因此,应在未来的试验中评估抗心律失常药和/或心脏复律是否对伴有AF的TTS患者有益。
原始出处:
Ibrahim El‐Battrawy.et al.Impact of Atrial Fibrillation on Outcome in Takotsubo Syndrome: Data From the International Takotsubo Registry.JAHA.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.119.014059
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












理学记器
98
#AHA#
47
#综合征#
66
#患者结局#
62
#Takotsubo#
75
房颤,临床上碰到很多哦
73
学习了
84