Cell Stem Cell:iPS细胞与核移植技术的优劣比较
2014-11-13 koo 生物360
立志做土豪的土鳖微宝纽约干细胞基因会研究所(NYSCF)的研究人员,对 iPS生成的多能干细胞和体细胞核移植(SCNT)生成的胚胎干细胞进行了深入比较,并将结果发表在本期的Cell Stem Cell杂志上。 研究人员发现,iPS和SCNT得到的细胞有着高度相似的基因表达和DNA甲基化模式,而且细胞出现了数量相当的DNA突变。这说明重编程过程本身就会引发突变,与使用哪种方法没什么
立志做土豪的土鳖微宝纽约干细胞基因会研究所(NYSCF)的研究人员,对 iPS生成的多能干细胞和体细胞核移植(SCNT)生成的胚胎干细胞进行了深入比较,并将结果发表在本期的Cell Stem Cell杂志上。
研究人员发现,iPS和SCNT得到的细胞有着高度相似的基因表达和DNA甲基化模式,而且细胞出现了数量相当的DNA突变。这说明重编程过程本身就会引发突变,与使用哪种方法没什么关系。
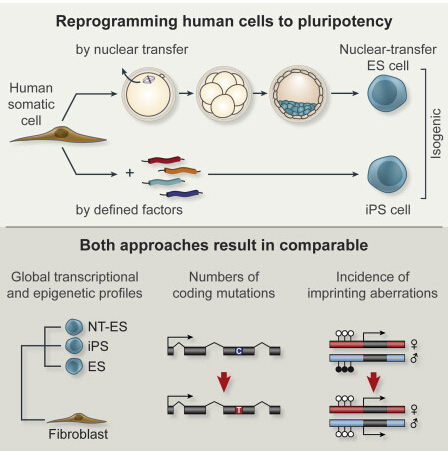
虽然iPS和SCNT都能生成多能干细胞,但它们的过程是完全不同的。iPS技术需要在成体细胞中表达几个关键基因,将细胞逆转到类似胚胎的状态。SCNT是用成体细胞的核替换卵细胞或卵母细胞的核,生成带有成体细胞遗传物质的胚胎干细胞。在理论上,不同方法生成的细胞应当带有不同的特性。今年早些时候NYSCF的科学家们通过SCNT成功生成了人类胚胎干细胞,再次引发了iPS和SCNT孰优孰劣的争论。
“我们的研究显示,生成患者自身干细胞现在有两种方法,它们都有潜力用于临床治疗。我们也为那些在iPS细胞上进行基础研究的科学家们带来了好消息。研究表明,在基因表达和DNA甲基化方面,这些细胞与人类胚胎干细胞非常相似。至于我们发现的突变对重编程的临床应用有何影响,这个问题将成为人们争论的焦点,”文章的资深作者Dr. Dieter Egli说。
在这项研究中,研究人员构建了来源相同的iPS和SCNT细胞系,比较了它们遗传编码的突变频率,并通过DNA甲基化和基因表达模式评估了它们与胚胎状态的相似度。研究显示,iPS和SCNT都能将已分化细胞有效重编程为干细胞,这两种方法生成的细胞在基因表达和DNA甲基化模式方面非常类似。
在遗传编码方面,SCNT和iPS细胞中的突变频率很接近。另外,这些细胞的印记基因也发生了数量相当的甲基化改变。从这些方面来看,SCNT和iPS可以说是半斤八两。
研究人员还研究了来自未受精人类卵母细胞的胚胎干细胞,和源自剩余IVF胚胎的胚胎干细胞。研究表明,SCNT和iPS细胞存在更多的异常。这说明,已分化的成体细胞重编程为干细胞存在着内在的缺陷,与诱导方法关系不大。
“我们还不清楚哪一种技术会生成治疗所需的最佳细胞,”NYSCF的CEO和创始人Susan L. Solomon说了。
Bjarki Johannesson9, Ido Sagi9, Athurva Gore9, Daniel Paull, Mitsutoshi Yamada, Tamar Golan-Lev, Zhe Li, Charles LeDuc, Yufeng Shen,Samantha Stern, Nanfang Xu, Hong Ma, Eunju Kang, Shoukhrat Mitalipov, Mark V. Sauer, Kun Zhang, Nissim Benvenisty, Dieter Egli. Comparable Frequencies of Coding Mutations and Loss of Imprinting in Human Pluripotent Cells Derived by Nuclear Transfer and Defined Factors. Cell Stem Cell, 6 November 2014; DOI: 10.1016/j.stem.2014.10.002
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Cell#
80
#CEL#
64
#stem cell#
66
#iPS#
57
#STEM#
76
#iPS细胞#
54