Cell子刊:宋红军、明国丽夫妇 寨卡病毒研究进展
2016-12-07 佚名 生物通
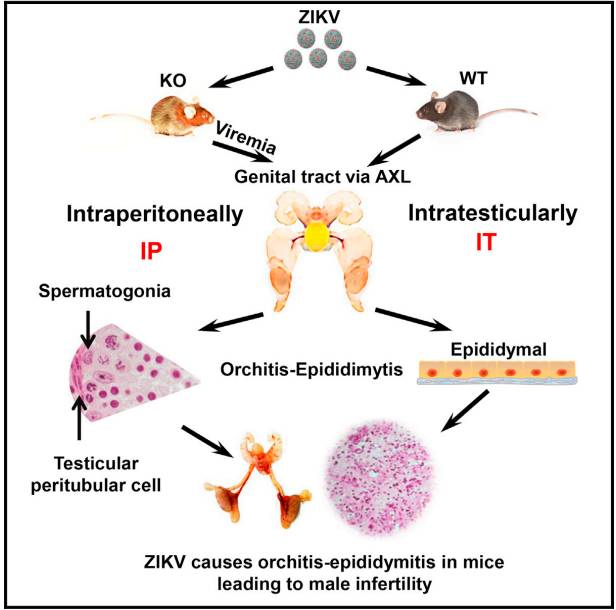
导语:12月1日,宋红军和明国丽与佛罗里达州立大学的Hengli Tang,在《Cell Stem Cell》杂志上合著了一篇题为“Advances in Zika Virus Research: Stem Cell Models, Challenges, and Opportunities”的综述文章,回顾了干细胞为基础的寨卡病毒研究的重要进展,并讨论了当前的挑战和未来的机遇。约翰霍普金斯大学医
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CEL#
56
#Cell#
60
#寨卡病毒#
56
#研究进展#
59
#寨卡#
70
科研界的夫妻档,哈哈?
83