NEJM:院前对脑卒中患者用硫酸镁保护脑神经
2015-02-19 MedSci MedSci原创
院前对脑卒中患者用硫酸镁保护脑神经 背景 硫酸镁应用于处于脑卒中发作潜伏期的患者身上已被证明是有保护神经的作用,并且若是在脑卒中表现初期使用则可以体现出硫酸镁潜在的功效和可被接受的安全性能。但是推迟启动脑神经保护药物的研发这一态度和观点已经阻碍了脑神经保护药物研发早期的三期临床试验的进展。方式 我们随机分配怀疑发生中风的病人为两组,让他们在脑卒中症状出现的2个小时内分别接受静脉注射硫酸镁或者

硫酸镁应用于处于脑卒中发作潜伏期的患者身上已被证明是有保护神经的作用,并且若是在脑卒中表现初期使用则可以体现出硫酸镁潜在的功效和可被接受的安全性能。但是推迟启动脑神经保护药物的研发这一态度和观点已经阻碍了脑神经保护药物研发早期的三期临床试验的进展。这项研究名为FAST-MAG(Field Administration of Stroke Therapy–Magnesium)临床试验(院前使用镁治疗卒中),结果发表于2月5日刊登在《新英格兰医学杂志》(New England Journal of Medicine)。2014年美国卒中协会(American Stroke Association)举办的国际卒中大会(International Stroke Conference)首次发布了这一研究的进展——对可疑卒中患者院前静脉注射硫酸镁急救,根据患者90天后残疾状况进行评判,该方法无效;但同时这一临床试验也证实,此类院前急救治疗措施是安全、可行的。
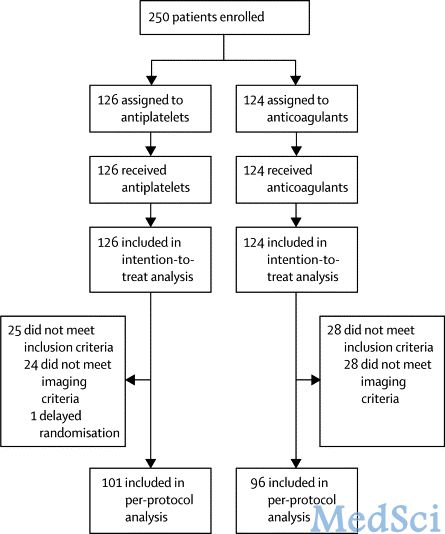
我们随机分配怀疑发生中风的病人为两组,让他们在脑卒中症状出现的2个小时内分别接受静脉注射硫酸镁或者静脉注射安慰剂,使用的剂量是以恒定的滴速从病人到达医院之前医护人员开始注射硫酸镁或者安慰剂起,至病人到达医院后一个24小时值班的静脉输液中心开始为病人输液进行治疗为止。实验的初步结果是病人因患病导致住院平均接受治疗的时间是90天。通过对病人使用改良的兰金量表进行评估疾病严重程度,用分数衡量以得出结果。(分数范围是从0到6,分数越高表明疾病程度更严重。)
研究人员通过两个步骤,从可疑卒中患者中筛选出符合试验标准的受试者。这一程序包括急救人员首先进行约1-2分钟的Los Angeles院前卒中筛查(Los Angeles Prehospital Stroke Screen),包含有8个项目;接着由医生通过无线电与急救人员对患者进行复查,以及患者本人或监护人法律上授权参与试验。
在参与该实验的1700名患者中,有857名患者接受了静脉注射硫酸镁,843名患者接受静脉注射没有任何作用效果只是起对照作用的安慰剂。最终诊断显示,73.3%的患者为缺血性卒中,22.8%的患者为颅内出血,同时3.9%的患者为类中风症状。从出现症状到或者治疗的平均时间为45分钟。
通过实验研究表明,在脑卒中症状出现最早的两个小时内使用硫酸镁是安全的、被认可的并且是可以保护脑神经的。但是在疾病治疗期间的90天内并没有明显改善疾病效果的作用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











不错耶.学习了
106
#脑卒中患者#
118
#院前#
86
#脑神经#
77
#卒中患者#
116
有参考价值
144
#硫酸镁#
98
到底是有用还是没用?
176