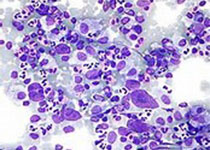
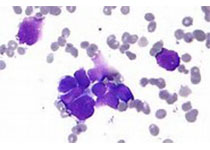
Brit J Cancer:SLC2A3介导的维生素C摄取减少会促进白血病的发生发展
2020-03-23 QQY MedSci原创
维生素C是一种能够参与表观遗传重塑的新型肿瘤代谢抑制剂,并提出其可以作为治疗白血病的潜在治疗策略。维生素C是TET酶(Tet甲基胞嘧啶双加氧酶)的辅因子,其可以调节TET的活性。
该研究旨在确定维生素C治疗的AML中的潜在的生物学标志物。
综上研究表明,SLC2A3可作为预测维生素C治疗AML效果的潜在生物标志物。
原始出处:
J Liu et al.Decreased vitamin C uptake mediated by SLC2A3 promotes leukaemia progression and impedes TET2 restoration. British Journal of Cancer
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








谢谢分享
100
#发生发展#
84
学习了很有用不錯
110
学习了,谢谢分享
115
学习
116