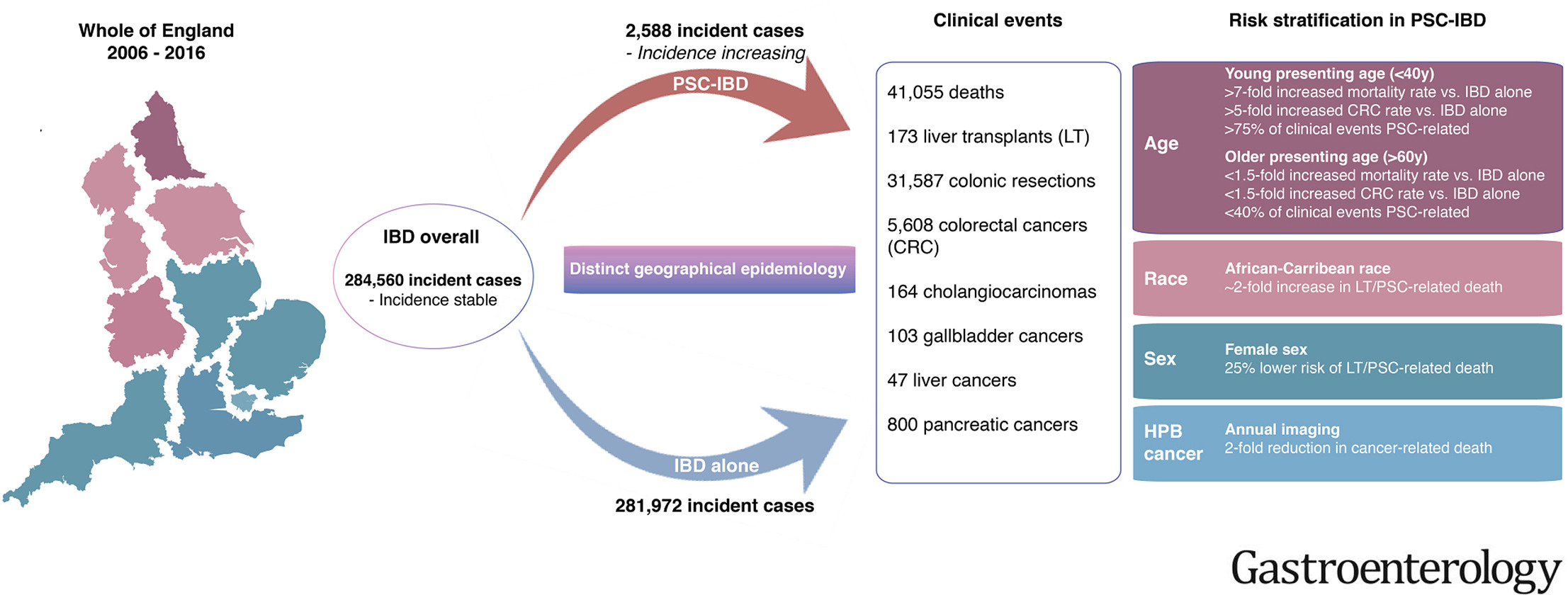
Gastroenterology:伴有原发性硬化性胆管炎的炎症性肠病患者的预后研究
2020-10-19 MedSci原创 MedSci原创
伴有原发性硬化性胆管炎的炎症性肠病患者其结肠癌、肝胰胆管癌和死亡风险增加。40岁及以下、男性以及非洲加勒比裔人群的预后较差。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#GAS#
95
#Gastroenterol#
55
#AST#
72
#原发性#
62
说的太好了
87
#原发性硬化性胆管炎#
82
#硬化性#
0
#Gastroenterology#
59
#炎症性#
56
#炎症性肠病患者#
88