Cell:大麻素受体三维精细结构揭密
2016-11-22 MedSci MedSci原创
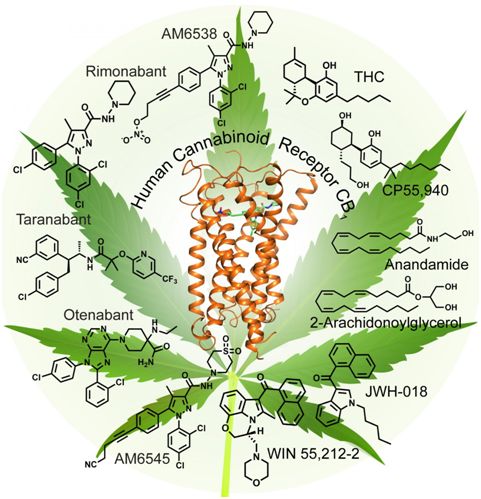
上个月,上海科技大学 iHuman 研究所的科研团队也成功解析了人源大麻素受体 (human Cannabinoid Receptor 1, CB1) 的三维精细结构,相关成果公布在Cell杂志上,研究主要工作在上海科大完成,iHuman研究所副所长、教授刘志杰,创始所长、特聘教授 Raymond Stevens 是论文的共同通讯作者。这一研究将有助于研发靶向这一受体的新治疗方法。本月11月16日
上个月,上海科技大学 iHuman 研究所的科研团队也成功解析了人源大麻素受体 (human Cannabinoid Receptor 1, CB1) 的三维精细结构,相关成果公布在Cell杂志上,研究主要工作在上海科大完成,iHuman研究所副所长、教授刘志杰,创始所长、特聘教授 Raymond Stevens 是论文的共同通讯作者。这一研究将有助于研发靶向这一受体的新治疗方法。
本月11月16日的Nature杂志上,德州大学西南医学中心的研究人员报告了结合并响应大麻化学成分的大脑受体:大麻素受体的最新三维结构图。文章的通讯作者是西南医学中心生物物理学和生物化学系副教授Daniel Rosenbaum博士。
大麻是当今西方社会滥用最多的成瘾性药物,但由于大麻对中枢神经系统有抑制、麻醉作用,因此也用于临床上,然而这种作用由于其副作用——损伤工作记忆(working memory,这是一种短暂时刻的知觉,一系列操作过程中的前后连接关系,后一项活动需要前项活动为参照,生物通注),因此倍受争议。
人源大麻素受体 (CB1) 是人类中枢神经系统中表达量最高的G蛋白偶联受体 (G protein-coupled receptor, GPCR)。CB1是大麻主要有效成分:四氢大麻酚 (∆9-tetrahydrocannabinol, THC) 的主要作用靶点, 是治疗疼痛、炎症、肥胖症以及药物滥用的潜在药物靶点。然而,由于长期以来缺乏 CB1 的结构信息,基于 CB1 的药物研发并不顺利。
上海科技大学的研究解析了CB1 与小分子拮抗剂 AM6538 复合物的精细晶体结构,分辨率为2.8埃。这一晶体结构揭示了 CB1 结合 AM6538 的复杂疏水结合口袋 (binding pocket)。AM6538 非共价的紧密结合模式使其具备了成为长效缓释药物分子的巨大潜力,这一特性也是治疗成瘾障碍药物的基本要求。此外,通过基于 CB1 三维结构的分子对接及动力学模拟分析,研究组还获得了不同类型的小分子激动剂与 CB1 的结合方式,揭示了配体小分子与 CB1 相互作用的新模式。
西南医学中心的这篇文章分辨率则达到了2.6 埃,Rosenbaum博士表示,“我们的结构显示了另外一种重要的结合口袋,也是科学家们药物研发的兴趣靶标之一。总体来说,这两个结构是互补的,但是我认为我们的结构能为了解大麻素,以及抑制剂如何与受体结构提供更好的框架。”
下一步Rosenbaum博士研究组希望能获得CB1与THC的结合结构。
原始出处:
Hua T, Vemuri K, Pu M, Qu L, Han GW, Wu Y, Zhao S, Shui W, Li S, Korde A, Laprairie RB, Stahl EL, Ho JH, Zvonok N, Zhou H, Kufareva I, Wu B, Zhao Q, Hanson MA, Bohn LM, Makriyannis A, Stevens RC, Liu ZJ. Structure of the Human Cannabinoid Receptor CB1. Cell. 2016 Oct 20;167(3):750-762.e14.
Shao Z, Yin J, Chapman K, Grzemska M, Clark L, Wang J, Rosenbaum DM. -resolution crystal structure of the human CB1 cannabinoid receptor. Nature. 2016 Nov 16. doi: 10.1038/nature20613
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CEL#
50
#Cell#
66
学习了,赞一下!
78
#大麻#
51
#大麻素#
62