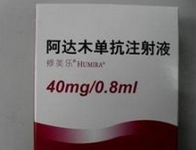
哪些类风湿关节炎患者阿达木单抗剂量可减半?
2016-03-09 佚名 环球医学
众多临床研究已证实,在类风湿关节炎的治疗中,阿达木单抗(ADA)具有显著的疗效,可有效改善症状和体征,抑制骨质破坏,并且能够改善身体机能。发表在《Rheumatology (Oxford)》的一项新研究表明,ADA剂量减半对于已经实现缓解和具有充足药物水平的患者来说是可行的。 本研究评估64名类风湿关节炎患者中,阿达木单抗剂量减半后对治疗效果、药物的体内水平的影响,以及研究在剂量减半后的第24周
众多临床研究已证实,在类风湿关节炎的治疗中,阿达木单抗(ADA)具有显著的疗效,可有效改善症状和体征,抑制骨质破坏,并且能够改善身体机能。发表在《Rheumatology (Oxford)》的一项新研究表明,ADA剂量减半对于已经实现缓解和具有充足药物水平的患者来说是可行的。
本研究评估64名类风湿关节炎患者中,阿达木单抗剂量减半后对治疗效果、药物的体内水平的影响,以及研究在剂量减半后的第24周能够预测患者达到持续缓解或最低疾病活动度最佳的阿达木单抗水平的折点。
抗ADA抗体水平由ELISA测定,ADA水平使用夹心酶联免疫吸附试验评估,通过DAS-28的变化评估治疗应答。通过接受者操作特征曲线分析预测持续缓解的药物最佳临界水平。
结果显示,基线时,分别有25(39.1%)和39(60.9%)名患者达到了持续缓解和LDA。24周ADA剂量减半治疗后,23人保持持续缓解,2人由缓解转变为LDA,24人持续LDA,15人疾病复发(23.5%)。3名患者在剂量减半后的24周体内出现了抗ADA抗体,体内药物浓度很低,且伴随疾病复发。其余61名抗ADA抗体阴性的患者中,24周的剂量减半治疗后,ADA水平降低了一半(中位5.5 vs 2.6μg/ml)。
持续缓解(中位10.5μg/ml)或LDA患者(4.5μg/ml)比疾病复发的患者(0.9μg/ml)的基线ADA水平明显更高,表明了ADA水平和治疗应答之间具有相关性。高于6.4μg/ml临界值的ADA水平提示患者在ADA剂量减半后依然可以达到持续缓解,并具有较高的敏感度和特异性。
ADA剂量减半对于已经实现缓解和具有充足药物水平的患者来说是可行的。治疗药物监测有助于临床医生优化接受抗TNF-α治疗的患者的剂量方案,并预防过度治疗。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#类风湿关节炎患者#
67
奶奶
137
#关节炎#
57
#类风湿#
66
#风湿关节炎#
54
#阿达木#
47