JACC:evolocumab治疗家族性高胆固醇血症的远期预后研究
2020-02-21 不详 MedSci原创
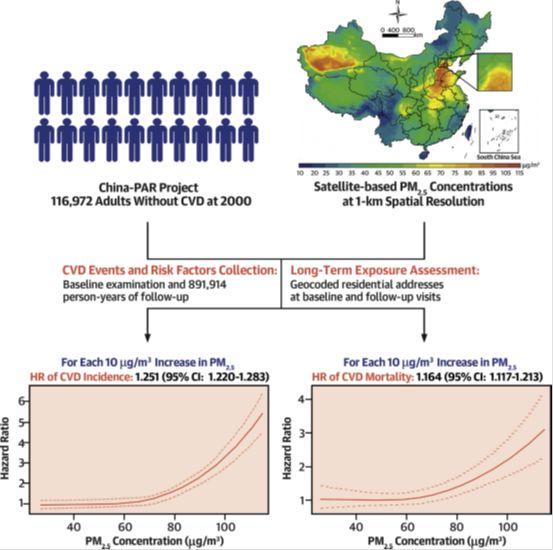
对不能达到低密度脂蛋白胆固醇(LDL-C)目标的家族性高胆固醇血症(FH)患者,前蛋白转化酶-枯草杆菌蛋白酶9抑制剂治疗是一种治疗选择。本研究的目的旨在评估evolocumab对纯合FH或严重杂合FH患者的远期有效性和安全性。本研究纳入分析了300名接受evolocumab治疗的患者(纯合FH为106名),经过平均4.1年时间的随访,有89.3%的患者发生了不良反应时间,最常见的是鼻咽炎、流感、上
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#mAb#
86
#JACC#
74
#远期预后#
70
#ACC#
80
#高胆固醇血症#
78
#Evolocumab#
81
#家族性#
65