Cell :改写教科书!新型免疫细胞或才是糖尿病关键!别再怪胰岛素啦!
2019-06-02 Ruthy 转化医学网
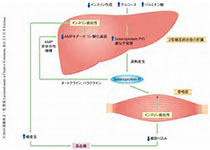
随着经济发展和人民生活水平的提高,全球范围内糖尿病的患病率飞速增长,流行普遍呈现年轻化、扩大化趋势,且目前尚无根治之法,只能以控制为主,故而已经成为人类健康的一个巨大挑战。目前普遍认为1型糖尿病与自身免疫息息相关,异常的自身抗体在胰岛素的驱动下损伤人体胰岛中分泌胰岛素的β细胞,使之不能正常分泌胰岛素是其发病的重要原因。近日,约翰霍普金斯大学的研究人员发现了一种新型免疫细胞——双表达细胞(DEs),
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
61
#Cell#
50
#胰岛#
48
谢谢MedSci提供最新的资讯
63
虽然距离改写还有一段距离,但是这个观念的确是一个变革
74