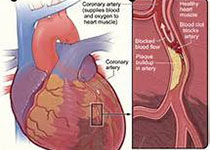
JACC:未经治疗的中重度主动脉瓣狭窄患者远期生存率低
2019-10-18 不详 MedSci原创
历史数据显示未接受治疗的主动脉瓣狭窄(AS)患者的生存率低主要局限于严重AS患者。本研究的目的旨在评估所有AS类型患者的预后。本研究纳入分析了测量过主动脉瓣流速和压差的122809名男性患者(平均年龄61±17岁)和118494名女性患者(62±19岁),并排除之前接受过主动脉瓣干预治疗的患者。最终,共有16129名患者(6.7%)、3315名(1.4%)和6383名(2.6%)患者分别为轻度、中
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JACC#
68
#重度主动脉瓣狭窄#
74
#生存率#
65
#ACC#
61
#主动脉瓣#
64
#主动脉#
50