Nature:重大突破!日本完成世界首例异体诱导性多能干细胞移植临床试验!:临床大发现
2017-04-01 应雨妍 奇点原创文章
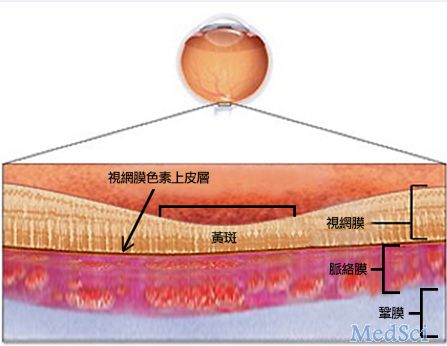
3月28日,一名60多岁的日本男子成为了世界上首个接受异体诱导性多能干细胞(iPSCs)移植的人!如果后续研究证明治疗取得了不错的效果的话,那么这毫无疑问是iPSCs临床应用的又一个里程碑,是iPSCs治疗走向标准化和通用化的重要转折点。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#世界首例#
75
#诱导性#
62
#Nat#
0
#细胞移植#
54
#日本#
66
不得不说,日本在iPSC这方面做的确实很好
72