NEJM:乳腺癌筛查指南更新——IARC观点
2015-06-09 姜缓缓 编译 中国医学论坛报今日肿瘤微信公众号
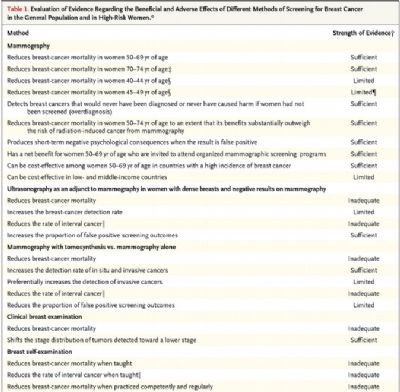
乳腺癌筛查的目的是通过对无症状女性进行早期检测,降低这种癌症的死亡率,以及与疾病晚期相关的发病率。使筛查的作用达到最大化的关键是早期获取有效的诊断和治疗。而筛查的综合质量是保持筛查利弊平衡的重中之重。 6月3日《新英格兰医学杂志》(New Engl J Med)在线发布国际癌症研究机构(IARC)乳腺癌筛查指南。IARC此次对其2002发布的乳腺癌筛查手册的更新主要基于以下几个方面原因。1.晚期
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















希望有更多更好指南
84
#IARC#
57
#指南更新#
62
好文
156
#乳腺癌筛查#
64
看看
160